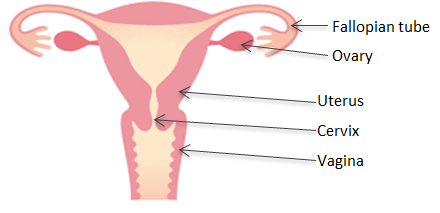
A hysterectomy is the removal of the uterus (womb) and usually the cervix (neck of the womb). Depending on the reason for hysterectomy, your surgeon will also discuss the additional risks and benefits of removing the tubes (salpingectomy) and ovaries (oophorectomy) with you. A hysterectomy is usually performed under general anaesthesia.
Why do I need this operation?
- Painful, heavy periods which have failed to respond to medical treatment
- Fibroids
- Prolapse of the womb
- Endometriosis
- Severe, recurrent or untreatable pelvic infection
- Abnormal cells in the womb including pre cancer and cancer of the womb
Types of hysterectomy and how it is performed
What is removed?
There are different types of hysterectomy and the one most suitable for you will depend on your individual symptoms and overall health.
Sub total hysterectomy
- What is removed?
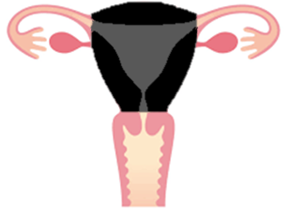
o Your Womb (in black)
- What is left behind?
o Ovaries, Cervix and Vagina
- What does this mean for you?
o You will not have periods (though a few women may have some spotting at the time of their periods coming from the top of the cervix)
o You will still require smear tests as you still have your cervix
o Your ovaries, which produce the female hormone oestrogen, are not removed
Total hysterectomy
- What is removed?
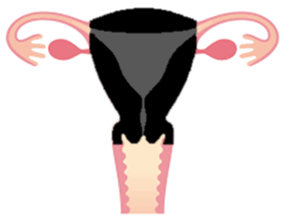
o Your Womb and Cervix (in black)
- What is left behind?
o Ovaries and Vagina
- What does this mean for you?
o You will not have periods
o You will no longer require smear tests unless specifically stated by your doctor
o Your ovaries, which produce the female hormone oestrogen, are not removed
Total hysterectomy bilateral salpingooophorectomy
- What is removed?
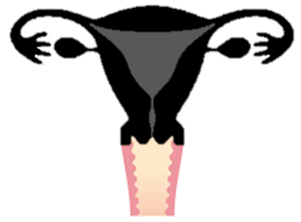
o Your Womb, Cervix, Tubes and Ovaries (in black)
- What is left behind?
o Your Vagina
- What does this mean for you?
o You will not have periods
o You will no longer require smear tests unless specifically stated by your doctor
o You will have your menopause (change) if it has not already taken place
How is a hysterectomy performed?
Abdominal
The womb is removed via a cut across the tummy. The cut may be horizontal, about 10-12 cm long and just above the pubic hairline. Occasionally a vertical (up and down) cut may be needed. The surgeon will discuss the planned incision prior to your operation.
Vaginal
The womb is removed through the vagina. The cuts are made on the inside of the vagina so you will not be able to see them.
Laparoscopic
This is a keyhole procedure with several small cuts on your tummy used to free the womb, which is then removed vaginally.
Your doctor will discuss the most suitable route for your hysterectomy with you.
The benefits
This depends on the reason for your surgery but benefits include:
- No more bleeding
- No more cervical smear tests (for some women)
- No more pregnancies, so no need for contraception
- Improvement in pain related to periods
The alternatives to surgery
This depends on the reason for which you are considering surgery. There may be alternatives if you are having your hysterectomy for painful or heavy periods, fibroids, prolapse or endometriosis. Discuss alternatives with your doctor to check if there may be another option available to you.
The risks
Hysterectomy is major surgery. 4 in every 100 (4%) women undergoing hysterectomy will experience a serious complication.
Frequent risks include
- Infection: is the commonest complication of hysterectomy occurring in between 2 to 10 women in every 100. Infection may develop in the skin, pelvis, bladder or chest and may require readmission to hospital or delay your discharge from the hospital.
- Bleeding: may occur in up to 4% of hysterectomies but less than 1% of women will require blood transfusion post- operatively. Optimising your pre-operative haemoglobin levels with iron supplements may help reduce the risk of needing a transfusion.
- Skin bruising or wound gaping.
- Abdominal/ pelvic or scar pain.
- Shoulder tip pain: may occur after laparoscopic hysterectomy due to the gas used to inflate the tummy during the procedure, irritating the diaphragm for up to 24 hours.
Serious risks include
- Injury to bowel, bladder, ureters (tubes connecting the bladder to the kidneys), nerves or blood vessels within the pelvis: These complications occur in up to 2 in every 100 women undergoing hysterectomy (2%). Laparoscopic hysterectomy is associated with a higher risk of injury to the bladder or ureters than an abdominal or vaginal approach. If you have had a laparoscopic or vaginal hysterectomy it may be necessary to perform a laparotomy (10-12 cm cut on the abdomen) to repair any damage to these structures.
- Developing a blood clot in the legs or lung: may occur in 1% of women undergoing hysterectomy. Your risk may be increased due to your age, other medical conditions, your weight and personal or family history of blood clots. Your surgeon will discuss this prior to your operation as well as discussing measures we can use to reduce this risk e.g. surgical compression stockings, mechanical leg compression in theatre and blood thinning medication (enoxaparin).
- Return to theatre due to bleeding or other complications: occurs in up to 1 in 100 (1%) women after hysterectomy. If you have had a laparoscopic or vaginal hysterectomy it may be necessary to perform a laparotomy (10-12 cm cut on the abdomen) if you return to theatre to gain access to fix the problem if the problem cannot be dealt with laparoscopically.
- Long-term disturbance to bladder function: is uncommon. It is more common if the hysterectomy is carried out at the same time as a pelvic floor repair (repair of prolapsed vaginal walls).
- Hernia: at site of abdominal incisions or laparoscopic port site occurs in up to 1 in 100 (1%) of women after hysterectomy.
- Ovarian failure: If the ovaries are conserved at hysterectomy in a pre-menopausal woman, there is a risk that she may undergo a slightly earlier menopause.
- Vault dehiscence: may occur in up to 4 women in every 1000 undergoing hysterectomy.
- Death: is rare after hysterectomy occurring in less than 2 in 10 000 women.
The operation
What happens before your operation?
You will be informed by post of a time to attend “Pre Admission Clinic”. This is usually several weeks before your operation. It allows us to ask you some general health questions, examine you and do some routine tests e.g. blood tests. It is also a good time for you to ask any questions about your anaesthetic but you will not be meeting the gynaecologist at this visit. Find out more information about this in the NBT Preoperative Assessment Clinic video:
You will be admitted to the gynaecology ward on the day of your operation and you will meet the gynaecology surgeon to finalise the consent form. You may also meet a physiotherapist on the ward.
What happens after your operation?
When you wake up you will be in the recovery room. You will usually have an oxygen mask on your face and a drip into the back of your hand.
You may also have:
- A tube in the bladder (a catheter) to drain the urine - this is possible for all types of hysterectomy.
- A gauze “pack” in the vagina - sometimes used after vaginal surgery.
- A wound drain (a tube coming from just next to the wound) - rarely used but most common for open surgery.
These tubes are usually removed in the first 24 hours.
What pain relief will I have?
- Paracetamol.
- Ibuprofen or Voltarol an anti-inflammatory painkiller
- Codeine based tablets
- Occasionally PCA pumps (patient controlled analgesia) which is a drip that contains painkillers like morphine
The recovery period
What should I expect during recovery?
- Usual length of stay in hospital
o You will be admitted to hospital on the day of your operation. You may be able to go home within 24 hours depending on how the surgery is performed. Most people stay in hospital for one to three days.
- After effects of general anaesthesia
o Modern anaesthetics are short lasting therefore you should not have after-effects for more than the day of your operation. During the first 24 hours you may feel more sleepy than usual and your judgement may be impaired. You are likely to be in hospital for this time, if not you should have an adult with you and you should not drive or make any important decisions.
- Stitches and dressing
o The cuts on your abdomen will be closed by stitches or glue. Glue and most stitches will dissolve by themselves. Other stitches will need to be removed by the practice nurse at your GP surgery in five to seven days after your operation. These cuts may be covered by dressings initially. You should be able to take this off about 24 hours after your operation and have a wash or shower.
o Stitches in your vagina will not need to be removed, as they are dissolvable. You may notice a stitch coming away after a few days or weeks; this is normal.
- Vaginal bleeding
o You can expect vaginal bleeding for one to two weeks after your operation. Some women have little or no bleeding initially, and then a sudden gush of old blood or fluid about 10 days later, which usually stops quickly. You should use sanitary towels rather than tampons.
- Pain and discomfort
o You can expect discomfort in your lower abdomen for at least the first few days after your operation. You may also have some pain in your shoulder. You should be provided with painkillers when leaving hospital. Some painkillers that contain codeine can make you sleepy, slightly sick and constipated.
- Your doctor will let you know when you can return to your normal activities.
When to seek medical advice?
It is quite unusual to have any problems once you are at home.
Please attend your nearest A&E if you experience any of these issues:
- Sudden feeling of shortness of breath or chest pain
- A temperature above 38°C
- Severe pain or increasing pain
- Nausea and vomiting
- Increased bleeding from your vagina (bright blood or clots)
- If you are unable to pass urine
- Pain, swelling or redness in your calf
Please see your GP if you experience any of the following:
- Constipation
- Wound pain or redness of your wound area
- Discharge from your wound
- Offensive smelling, itchy, yellow/green discharge from your vagina
- Burning pain or discomfort when passing urine
Further information
