The page has information about caring for your relative/friend at the end of life.
The doctors and nurses looking after your relative/friend believe that there has been a change in their condition indicating that they are dying and are now in the last hours, days or weeks of life. This can be an extremely distressing and worrying time for everyone.
At North Bristol NHS Trust we want to be able to support you and your relative/friend as best we can. We are committed to providing high quality end of life care, which includes addressing pain and other symptoms, providing care in a way that ensures the privacy and dignity of your relative/friend, and by keeping everyone up to date about any changes in their condition or treatment.
Whilst the dying process is individual and we can’t always predict what will happen, there are some signs and symptoms that help us to recognise that someone is approaching the end of their life. This page aims to answer some of the questions you may have about your relative/friend’s care and what to expect when someone is dying.
What will happen next?
At North Bristol NHS Trust, we record the care given each day using a document called “The Purple Butterfly” framework which prompts staff to think about the individual needs of each person, ensuring that the most important aspects of care are addressed.
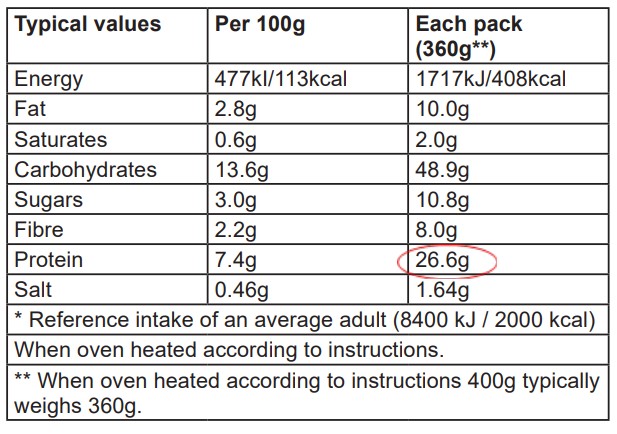
Non-essential medications, routine tests, and observations such as blood pressure monitoring are reviewed and usually stopped at this time. Instead, any symptoms your relative/friend may experience such as pain, nausea, breathlessness and restlessness will be reviewed regularly and changes will be made to their care as needed.
You and your relative/friend (if they are able) will be involved in the discussion regarding their care with the aim that you all fully understand the reasons why decisions are being made.
If your relative/friend’s condition improves then their plan of care will be reviewed and changed. All decisions will be reviewed regularly by the ward team. We will ask for the contact details of a named person so that we can keep you informed of any changes.
What documentation is used?
A symptom observation chart will be outside the room for staff to record any issues such as pain or distress that require intervention or medication from the doctors or nurses. The doctor will prescribe pain relief and other symptom-relieving medication on your relative/friend’s medication chart.
A purple butterfly sign will be placed on your relative/friend’s door as a way of communicating with all those involved in their care that they are in the last few days of life.
What can we expect during the dying process?
The dying process is unique to each person but in most cases there are signs which help to indicate that a person is dying, particularly when there has been a deterioration despite treatment in hospital.
Diminished need for food and drink
As someone becomes weaker and more unwell their appetite is likely to naturally reduce and eating and drinking become more difficult. Your relative/friend will be supported to take food and fluids if they so wish as long as they can safely do so; the treating team will guide you when this may no longer be possible.
Fluids via a drip are usually not needed when someone is dying, but it can be incredibly hard to see those we love not eating and drinking or receiving fluids.
The nursing team can show you how to give mouthcare to your relative/friend to help relieve any sensation of dryness or thirst. We urge you to ask the medical team if you have any questions or concerns about food and fluids.
Changes in breathing
People who have suffered with breathlessness for a long time are often concerned that they will struggle with breathing at the end of their life. However, the effort of breathing may become easier as they become less active and the need for oxygen decreases. For others, their breathing may become more shallow and rapid and they may find the sensation distressing. Breathing difficulties can be made worse by feelings of anxiety and this is often relieved by knowing that someone is close at hand. There is also medication that can be given if we feel someone is experiencing distress with their breathing.
Sometimes people have a build-up of secretions in the back of the mouth which can cause a noisy rattle because they can no longer cough and clear the secretions. If this develops, your relative/friend may be given medication to reduce it and changes in position may help. Noisy breathing is not always improved by medication or a change in position and although it can be distressing to hear, it is not distressing for the dying person.
Withdrawing from the world
This is a gradual process. Over a period of time, your relative/friend may spend more time sleeping and will often be drowsy when awake. This lack of interest in their surroundings is a natural process. Eventually they will lapse into unconsciousness, sometimes for a surprisingly long time.
When death is close their breathing pattern may change. It can sometimes appear more laboured and sometimes there are long pauses between breaths. This is normal and is not distressing to the dying person.
What else should we expect to happen during this time?
Medication and other treatments
Medication will be reviewed and anything that is no longer helpful may be stopped. New medication will be prescribed so that if a symptom occurs it can be addressed. Medication may be given as a small injection under the skin or as a continuous infusion using a syringe pump if it becomes difficult to swallow medication. If your friend/relative normally takes pain relief then this will be continued or given in an alternative way, usually via a syringe pump.
The staff will talk to you about the best way to maintain comfort by such things as looking at the position in bed, the use of a special mattress and mouth care. If your relative/friend is breathing through an open mouth, it is likely to become dry, so regular moistening and application of lipsalve will give comfort.
Spiritual, cultural and religious care needs
The team will wish to identify whether your relative/friend or you have any religious, cultural, or spiritual wishes, and if there are any particular things that may be important at this time. Please let staff know if you have any special requests or wishes relating to the moment of death or after death so that they can ensure that these are carried out .
You may be asked if either of you belong to a faith or community. If you do, you may wish for the staff to contact a faith leader from that community for support now or at the time of death.
You are welcome to meet a member of the hospital Spiritual/Pastoral Care Team (Chaplains phone number: 0117 414 3700). They are skilled people who can provide support even if you do not have a religious belief. They can be asked to visit and talk to you about any needs, fears, and worries.
How else can I help my relative/friend?
Don’t underestimate the importance of being with your relative/friend, even if you feel you aren’t doing much. Talking to your relative can help, even if they appear to be asleep. Telling them news from home, reading a book or the newspaper may be comforting to them, even though they may not be able to respond .
Please feel that you can hold your relative/friend‘s hand and touch them.
It is sometimes possible to help with some simple aspects of care - moistening their mouth, providing them with a drink or brushing their hair, for example. Please feel free to speak with a member of staff if you are unsure or would like some guidance.
This is a difficult time. Do not forget to take care of yourself. Visiting can be a very stressful and tiring time. Do take breaks from the bedside, try to get some rest and eat well. There are quiet spaces available for you to use on the wards. Please ask the staff to show you where they are located.
What happens after my relative/friend has died?
The ward staff can go through this with you and there is a separate leaflet explaining everything that needs to happen.
What other support is there for me?
The Sanctuary / Chaplaincy
The Sanctuary is located at Gate 30 and offers a place for quiet, reflection, meditation, prayer, and worship. It is for people of any or no faith and is open for patients or visitors at any time.
Purple Butterfly Volunteers.
Our Purple Butterfly volunteers are available most weekdays to offer an extra layer of support to you and your relative/friend. They can sit and listen to you and your relative/friend, offer you refreshments and provide short periods of respite should you wish to take a break from being at the bedside.
We can provide relatives/friends with a carers badge which allows access to the staff canteen (Vu, Level 5) giving you access to wider variety of hot food and drinks. The nursing team and Purple Butterfly volunteers can help you with this.
For information about food and drink facilities in the Brunel building visit:
Cafes & Shops | North Bristol NHS Trust (nbt.nhs.uk)
Parking
Parking permits are available, please discuss this with the ward team. This will need to be taken to the security and parking office at the main entrance on Level 1 for authorisation.
Pay and display charges apply 24 hours a day, 365 days of the year.
Parking Administrator Telephone: 0117 414 3335
Information/Communication
The team will be making regular assessments of your relative/friend’s condition. If you have any worries or concerns in between assessments, or at any time, please do not hesitate to let one of the doctors or nurses know. Being with someone at the end of their life can feel lonely and painful, so the staff are also here to offer you guidance, comfort and support.
If further support or symptom control is needed, the ward team will contact the Palliative Care Team:
Phone: 0117 414 0519
Monday–Friday 9am-5pm
© North Bristol NHS Trust. This edition published January 2024. Review due January 2027. NBT002815.