A pleural vent is a medical device that is used to treat a pneumothorax. This page will explain what a pleural vent is, why it is used and how it is inserted.
Why do I need a pleural vent?
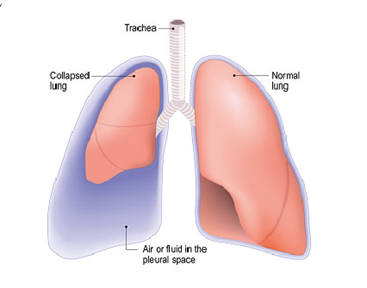
A pneumothorax occurs when air gets trapped in the space between the lung and the chest wall (the pleural space). The air gets there either from a defect on the surface of lung or through the chest wall. The air can squash the underlying lung and cause it to collapse.
You may experience some or all of the following symptoms; breathlessness, cough, or a sharp, stabbing pain on one side of the chest, which may be worse when breathing in.
There are different ways to treat a pneumothorax depending on the cause, how large it is and how severe your symptoms are. This includes conservative management (observation only), pleural aspiration and an intercostal chest drain. Your doctor will explain the benefits and risks of these options to you in more detail.
Sometimes, we can use a pleural vent instead of an aspiration or a chest drain.
What is a pleural vent?

A pleural vent is a small medical device. It consists of a small tube connected to a one-way valve inside a chamber. The tube sits inside the chest and the chamber sits on the front of the chest.
The pleural vent allows air to escape from the pleural space through the device to help the lung reinflate.
Unlike a chest drain, you can usually go home with a pleural vent in place and do not have to stay in hospital. The pleural vent stays in for a few days until the pneumothorax has healed.
How will the pleural vent be put in?
The pleural vent is inserted in hospital by a doctor who will talk to you about the benefits and risks of the procedure and ask you to sign a consent form.
You must tell the doctor if you take any medications that thin your blood, such as warfarin, apixaban, rivaroxaban or clopidogrel. These medications can increase the risk of bleeding and may need to be stopped before the procedure.
The procedure takes about 15 minutes, and you will be placed into a comfortable position on your back on a couch. Then:
- The insertion area is cleaned with an antiseptic to kill any bacteria on your skin. This may feel cold.
- Local anaesthetic is injected into the area with a small needle to numb the skin. This will feel sharp and you may feel a stinging sensation when the anaesthetic is injected.
- When the area is numb, a small cut is made and the pleural vent is inserted. This should not be painful but you may feel some pushing or pressure.
- The pleural vent is held in place on the front of your chest with a sticky dressing, and sometimes a stitch if needed.
- The blue disk at the top of the pleural vent will move up and down when you breath in and out, showing that it is working correctly.
What are the benefits of a pleural vent?
A pleural vent is simple and quick to insert with local anaesthetic, it allows continuous drainage of air from the pleural space, unlike an aspiration, and you can walk around as normal. If you feel comfortable, you may be able to go home with the pleural vent in place.
What are the risks of a pleural vent?
Inserting a Pleural Vent is a routine and safe procedure. However, as with any medical procedure, there are potential risks:
- Pressure or discomfort when the tube is inserted (common). The use of local anaesthetic reduces this discomfort. As the anaesthetic wears off you may notice the Pleural Vent more.
- Significant bleeding (very rare, around 1 in 500 for a chest drain). Inserting the tube may cause bleeding outside the skin or into the pleural space. If it is significant, you may need a further procedure to stop the bleeding or a blood transfusion.
- Damage to the lung or other nearby organs (very rare). This risk is reduced by checking a chest x-ray or sometimes using an ultrasound machine to confirm the position of the pneumothorax before the device is inserted.
- Re-expansion pulmonary oedema (very rare). This happens when a collapsed lung re-opens too quickly and fills with fluid. This can make patients feel more breathless and unwell. If this happens you may need to stay in hospital and be given oxygen.
- Discomfort whilst the pleural vent stays in (common). This is usually mild and can be relieved with simple painkillers such as paracetamol or ibuprofen.
- Skin reaction to the dressing. You should tell the doctor if you have had problems with dressings before.
- Infection around the skin or in the pleural space (rare, around 1 in 50 for chest drains). This is minimised by cleaning the skin effectively before device insertion and ensuring the Pleural Vent is kept clean and dry while it is in place.
- Tube becomes kinked or blocked and stops working. If this occurs, you may notice worsening breathlessness or chest pain.
- Swelling around the device. If air from the pleural space drains under the skin instead of through the device (because the device is blocked or no longer sitting in the right place), a problem called subcutaneous emphysema can develop. If you press on the swelling it feels crackly or crunchy, or like bubble-wrap. If it is mild and not worsening, it may not require any further action. However, if it spreads or worsens, you should arrange to be seen quickly (see below).
How do I look after the pleural vent at home?
Call 999 or attend the Accident and Emergency Department immediately if:
- The pleural vent comes out for any reason.
- You experience severe or worsening pain or breathlessness.
- You notice swelling around the device that is spreading rapidly.
Do check that the blue disk at the top of the Pleural Vent moves up and down when you breathe.
Do tell the nurses or doctors, using the contacts below, if the disk stops moving. This may mean the pneumothorax has resolved.
Do avoid heavy lifting, straining or vigorous exercise as this may displace the device or make the pneumothorax worse.
Do not take a bath, go swimming, or immerse the device in water. This can damage the device or dressing and increases the risk of infection.
Do not remove the device yourself.

Fluid collection chamber
Sometimes, fluid can come out of the chest in addition to air. The Pleural Vent can collect a small amount of this fluid in the chamber but may need to be drained periodically. If you notice the fluid collection chamber is full, please contact us using the numbers below.
How is the pleural vent removed?
The pleural vent must only be removed by a trained healthcare professional. Any dressings or stitches will be removed and then the device is pulled out. A simple dressing is placed over the area. This only takes a couple of seconds and is not painful. After it is removed, a chest X-ray will be repeated.
We will remove the pleural vent in the Pleural Clinic when the pneumothorax is resolved.
Who do I contact for more advice or help?
If you are an NBT patient and have queries or problems with your pleural vent device Monday to Friday 8am to 4pm, please contact:
Pleural Clinical Nurse Specialist Anna Morley 0117 414 1900
Respiratory Secretary Louise Brennan 0117 414 6451
In an emergency, please go directly to the Emergency Department.
© North Bristol NHS Trust. This edition published June 2022. Review due June 2025. NBT003482.
