What is gestational diabetes (GDM)?
Gestational diabetes (GDM) is high blood sugar (glucose) developed during pregnancy and usually disappears after giving birth (post-delivery). It can happen at any stage of pregnancy but is more common in the second or third trimester. It happens when your body cannot produce enough insulin – a hormone that helps control blood sugar levels – to meet your extra needs in pregnancy.
Key features of GDM:
- Insulin resistance is due to an increase in circulating hormones that cause glucose levels to rise.
- It is usually temporary – post-birth your hormone levels return to normal and blood glucose levels fall
- In some cases, post-birth blood glucose remains high – this can be type 2 diabetes.
- You will have an increased risk of type 2 diabetes later in life.
Why did I get GDM?
Any woman can develop gestational diabetes during pregnancy, but you have a higher risk if:
- You are over 40.
- You have a raised BMI (above 30).
- You have South Asian, Black Caribbean, African or Middle Eastern heritage – certain ethnicities have a higher risk.
- There is a family history of diabetes (one of your parents or siblings has diabetes).
- You had gestational diabetes in a previous pregnancy.
- You have polycystic ovary syndrome (PCOS).
- You have had a previous baby over 4kg.
Some women with no risk factors at all will also develop GDM. The key message is that GDM can happen through no fault of your own but there are lots of things you can do to help manage it.
What are the risks associated with GDM?
Most women with GDM have otherwise normal pregnancies with healthy babies. However, gestational diabetes can cause problems such as:
- Your baby growing larger than normal. This may lead to difficulties during the delivery (shoulder dystocia) and increases the likelihood of needing induced labour or a caesarean section.
- Small increased risk of stillbirth, though this is rare.
- Intrauterine growth restriction (when baby does not grow as big as it should).
- Pre-eclampsia – this is a condition that causes high blood pressure during pregnancy and can lead to complications if not treated.
- Polyhydramnios – this is when there is too much amniotic fluid (the fluid that surrounds the baby) in the womb, which can cause premature labour or problems at delivery.
- Risk of lower blood sugars (hypoglycaemia) in your newborn baby.
How is it monitored and treated?
If you have gestational diabetes, the risks associated with GDM can be reduced by controlling your blood sugar levels.
You’ll be given a blood sugar testing kit and asked to test a minimum of four times a day. The instructions are included and you will be sent links to the Agamatrix user video.
Blood glucose targets:
- Fasting: 3.5-5.2mmol/l
- 1 Hour after meals: 3.5-7.7mmol/l
When should I be concerned?
- More than 3 readings out range in 48 hours.
- More than 2 high readings on waking over 1 week.
What should I expect during pregnancy?
- Testing your blood glucose levels 4 times a day.
- Dietary changes.
- Medications is sometimes required (metformin tablets/insulin).
- Appointment and scan in GDM clinic every 4 weeks.
- Support from diabetes midwives on 0117 4141 072
- Induction of labour/elective caesarean section/delivery suite birth usually recommended.
- Colostrum harvesting recommended from ~36/40.
What happens after birth?
- You will stop diabetes medications (unless advised not to).
- Postnatal (after the birth) stay in hospital of at least 24 hours.
- Test your blood glucose levels for first 24 hours. It is useful to bring your blood glucose testing kit in from home so you are able to test your blood sugars when on the ward.
- Early first feed and skin to skin contact.
- Baby observations and blood glucose tests (every 3 hours until 2 normal readings).
Long term effects of gestational diabetes
Gestational diabetes normally goes away after birth. But woman who have had it are more likely to develop:
- Gestational diabetes again in future pregnancies.
- Type 2 diabetes.
You should have a blood test to check for diabetes 13 weeks after giving birth, and once every year after that if the result is normal.
See your GP if you develop symptoms of high blood sugar, such as increased thirst, needing to wee more often than usual, and a dry mouth, losing weight, repeated thrush, slow healing wounds– do not wait until your next test.
You should have the tests even if you feel well, as many people with diabetes do not have symptoms.
There is a type 2 prevention programme which your GP can refer you to or you can self refer to.
Healthy eating with gestational diabetes
A healthy diet is an important part of a healthy lifestyle at any time but especially for women who are pregnant or planning a pregnancy. What you eat and drink plays a key role in managing your blood glucose levels during pregnancy when you have GDM. The right balance of a variety of food is also important to make sure you and your developing baby get the nutrition you both need.
We base our healthy eating advice around the Eatwell guide, which you can find links to below. The Eatwell Guide divides the foods and drinks we consume into five main groups. Cultural and ethnic versions of the Eatwell Guide have been created which include foods commonly eaten in African and South Asian communities. Try to choose different foods from each of the food groups to help you get a wide range of nutrients that your body needs to stay healthy and work properly.
After monitoring glucose levels, the second step for managing gestational diabetes involves looking at your diet and exercise and making changes where possible to help control your blood glucose levels.
Planning your meals
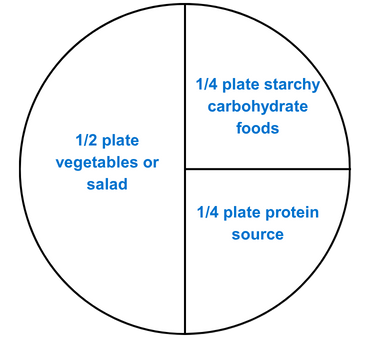
We recommend you base your meals around the portion plate model which is pictured below. This includes half a plate or vegetables or salad, a quarter of a plate of starchy carbohydrate foods, and a quarter of a plate of protein.
Counting the amount of carbohydrates in your meals is not usually necessary, however if you find it helps, here is a guide, per meals:
- Breakfast: 20g
- Lunch: 40-50g
- Evening meal: 40-50g
- Snacks: 15-20g or carbohydrate free
Note: This is just a guide, everyone has different degrees of insulin resistance with their GDM. By regular blood glucose monitoring you’ll be able to adjust your diet as you need to.
Carbohydrates
Carbohydrates have the biggest impact on our blood glucose levels. Your body breaks down carbohydrates into glucose (sugar).
It is important to not cut these foods out completely as they are the main source of energy for your body and your growing baby. They also provide important vitamins and can be a source of fibre.
You can eat all types of carbohydrate, but some will raise your blood glucose levels more than others, even when an appropriate portion size is eaten. Try to eat more of the higher fibre/low GI carbohydrates, as per the table below.
Our starchy carbohydrates are foods within the yellow section of the Eatwell guide. Examples include:
- Bread
- Pasta
- Noodles
- Rice
- Flour
- Cereals
- Plantain
- Yam
- Dosa
- Polenta
- Oats
A note on breakfast cereals
Many women find that breakfast cereals cause blood glucose levels to rise too much and must avoid them completely during pregnancy.
Try a lower carbohydrate breakfast such as natural or Greek yoghurt with one portion of fruit or eggs/avocado/cottage cheese, with one slice of seeded bread.
Glycaemic index
All food that contains carbohydrate have a glycaemic index value (GI). This is the speed that the body breaks down carbohydrate into glucose and absorbs it into the blood.
Low GI foods are the best choices as they are absorbed and raise the blood glucose more slowly so can help to keep your blood glucose levels within the target range and regulate your appetite much better. High GI foods are absorbed quicker and raise the blood glucose quickly.
Therefore we recommend that you try and choose foods from the Low GI food list.
The table below shows you some examples of low and high GI foods.
| Refined carbohydrates to avoid (High glycaemic index (GI)) | Try instead (Low glycaemic index (GI)) |
|---|---|
All white breads:
|
|
Low fibre and sugar coated breakfast cereals:
|
|
Rice, pasta, grains:
|
|
Processed potato products:
|
|
Fruit and vegetables
- These are the other largest section in the Eatwell guide. They give us a wide range of vitamins, minerals and fibre.
- Choose a variety of different coloured fruit and vegetables as they contain different combinations of important nutrients our bodies need to stay healthy.
- We encourage you to bulk out meals with vegetables or salad items as these are low GI and help fill you up at mealtimes whilst increasing our overall vegetable intake.
- It is important to moderate fruit intake as their natural sugar content directly affects our blood glucose levels and so we therefore recommend you limit fruit intake to 2-3 portions per day and to spread these portions out over the day.
- You can combine a fruit snack with some protein food such as natural yoghurt, a cube of cheese or a handful of nuts or seeds (see protein section below) which will help in preventing a rise in glucose.
- One portion of fruit is the size of your palm for example:
- One handful of berries.
- One small- medium apple, orange or pear.
- Two smaller fruits such as a plum, satsuma, or one ‘fun’ size banana.
- We recommended avoiding melon, pineapple, or papaya.
- Avoid fruit juice and fruit smoothies. If using tinned fruit avoid ones in syrup and drain off the juice.
- Fresh and frozen vegetables are equally as beneficial.
Protein
- Protein is an important nutrient in the diet. It plays a key role in muscle repair and development. High protein foods can also be a good source of iron, other vitamins and minerals, and omega 3.
- Foods that are high in protein include all meat, fish, eggs, beans, pulses, tofu, meat substitutes, nuts and dairy. When unprocessed, these high protein foods by themselves do not directly affect your blood glucose levels. When added to carbohydrate containing foods can actually reduce the impact on your glucose levels
- Most people in the UK easily meet their protein requirements if they have a protein portion at 2-3 meals per day. A portion of protein is equivalent to the palm of your hand or the size of a deck of playing cards.
- For general health, weight, and glucose, it is important to:
- Opt for lower fat cuts of meat where possible
- Limit your intake of processed and cured meats.
- Remove any of the visible white fat from meat, or skin from poultry.
- Try to use healthier cooking techniques like grilling, dry roasting, boiling or poaching rather than frying.
- White fish is a good source of lean protein. Oily fish such as salmon, trout, mackerel and herring provide the beneficial omega 3 fats. Pregnant women should eat no more than 2 portions of oily fish per week. Tuna does not count as oily fish but should also be limited to 4 medium-size cans per week. More information on food safety during pregnancy can be found on the NHS website – link to website in ‘other useful links section’.
Dairy
- Dairy foods are important within a healthy diet as they are a key contributor of calcium which is important for making strong bones and teeth. They are also a key source of iodine which is important for your baby's neurological (brain) development.
- Examples of dairy foods includes cows’ milk, yoghurts and cheese.
- If you don’t eat dairy due to personal choices, or due to allergy or intolerance, then it is important that you ensure your dairy alternatives are fortified with calcium and iodine.
- Aim for 3-4 servings of dairy per day to meet your calcium and iodine requirements. Examples of a portion include
- 200ml of milk, a 125g pot of yoghurt.
- 30g of cheese.
- For non-dairy sources portions may need to be larger.
- Additionally, dairy foods can be high in fat, and in particular saturated fats. So it is important to be mindful of our portion sizes and consider lower fat varieties where possible.
- It is important to be aware that milk contains a natural sugar called lactose and drinking large amounts of milk can have an unhelpful effect on glucose levels. However, adding small amounts of other dairy products to carbohydrate-containing foods can help to reduce the impact on glucose levels.
- For example, having a tablespoon of Greek yoghurt with your berries, or having a small chunk of cheddar cheese with an apple as these add additional protein.
Fats
Fats are needed in the diet as they play an important role with different aspects of health. Such as providing energy, warmth, protection of the internal body and key fat-soluble vitamins. However, it is important to note that all fats are very high in calories which can contribute to unhelpful weight gain.
Examples of food sources that are high in fats include:
- Oils.
- Butter.
- Spreads.
- Avocado.
- Nuts.
- Seeds.
- Cheese.
- Cream.
- Processed foods like cakes, biscuits, chocolate, pastry items and crisps.
We generally don’t need to deliberately add high fat foods into our diet as most people get enough fats within their normal diets. However, it is appropriate to try to keep our intake of high fat foods to 2-4 portions per day. Examples include a tablespoon of oil or butter, half an avocado, or 20g of nuts.
All fats are high in calories, but not all fats are the same in other ways, such as their impact on cholesterol level. It is important for everyone to try to limit their intake of saturated fats, such as those from animal products, and swap to unsaturated fat where possible, such as those in nuts, plant based oils and avocado.
Foods high in free sugars
Free sugars are sugars added to food such as in cakes, biscuits, chocolate and desserts. They are also naturally in honey, syrups and unsweetened fruit juices. However, the term free sugars excludes lactose in milk and milk products, and the sugars in whole fruit.
All sugars are a form of carbohydrate and therefore provide a rapid source of energy for our body, but foods high in free sugars often provide very little other nutritional benefit.
Free sugars also have a very quick impact on our blood glucose levels. This is normally unhelpful and pushes the levels above the target ranges unless our blood glucose levels are too low to start . It is important to reduce your intake of free sugars as much as possible, including in drinks.
Hydration
- Aim to drink 11-12 cups (200ml cups) (2.3L) a day. There is 300ml increase in how much fluid you need per day during the whole of pregnancy.
- Avoid drinks high in sugar: full sugar fizzy drinks and squash, energy drinks, fruit juice and smoothies.
- Current NHS guidelines on caffeine: no more than 200mg/day.
- This equals 2 cups of instant coffee or tea/day. Caffeine is also found in energy drinks, cola and chocolate. More information on this can be found on the NHS website.
Exercise in pregnancy
- Exercising during pregnancy has many benefits, including reducing stress and anxiety, improving sleep patterns.
- Exercise can also help your insulin work more effectively, which keeps your blood glucose level under control, especially walking or being more active post eating.
- We recommend trying to remain active for at least 15-20mins straight after eating; this can be going for a short walk or just being active around the house.
For more information on this please check: Exercise in pregnancy - NHS
Weight gain during pregnancy
Weight gain is generally inevitable during pregnancy due to all the physical changes that happen to help your baby grow and develop, but it is important to try not to gain too much weight throughout your pregnancy, particularly if you were overweight before.
- As mentioned previously, you do not need to eat for two and it is only in your last trimester when you need just 200 extra calories per day.
- It is also important not to follow an overly restrictive diet as this could harm you and your baby. Focus on making small changes to your diet, such as those discussed earlier on this page and keeping physically active.
Food safety in pregnancy
There are certain foods that are best to avoid while you are pregnant as they can put your baby’s health at risk. These include some types of cheese and raw or uncooked meat. For more details, please see websites below.
Meal pattern
Try to eat regular meals (breakfast, lunch, and evening meal). Spread your intake over the day to help to manage your blood glucose levels.
If you skip meals, you might be more likely to overeat at the next meal or end up on snacking on things that can have a big impact on your blood glucose.
Avoid eating carbohydrates late in the evening. Having your dinner too late at night can affect your fasting blood glucose the next day. If you can, try to have your dinner 2-3 hours before you go to bed. If you need to snack after dinner, opt for low carb options like nuts, cheese or a small portion of Greek yogurt.
Menu planning ideas (choose one from each section)
Breakfast:
- Rye/granary toast with eggs/nut butter/egg/cheese/ham/marmite.
- 20-30g Jumbo oats with skimmed milk or Greek yoghurt and seeds/nuts.
- Plain natural or Greek yoghurt with a handful of berries/nuts and seeds.
- 1 small chapatti made with wholemeal flour with dhal or meat/fish curry.
Mid-morning snack:
- 1x Ryvita with peanut butter/cottage cheese/cream cheese/cold meat.
- 1x portion of fruit.
- A small pot of natural or Greek yoghurt.
- Small handful (30g) of plain popcorn.
Lunch:
- A sandwich (1-2 slices of wholemeal granary bread) containing salad and a protein choice such as tuna/egg/cheese/meat.
- ½ a jacket potato with protein topper and salad on the side.
- Omelette with salad and a granary roll.
- 2-3 tablespoons of cooked basmati rice with meat/fish or vegetarian curry (avoid adding potato to the curry).
- 1 medium chapati with meat/fish or dhal and salad.
- 2 small samosas with plenty of salad and plain yoghurt.
Mid-afternoon snack:
- Veggie sticks and hummus.
- Sugar free jelly.
- Handful of nuts.
- A piece of fruit with a cube of cheese.
- 1 small samosa.
Evening meal:
- Stir fry bulked out with vegetables and meat/fish and 2-3 tablespoons of cooked basmati rice or noodles.
- 1 medium chapati and curry (meat/fish/lentils) and salad.
- Roast meat with vegetables and 3 egg sized potatoes (avoid Yorkshire pudding and stuffing or swap out for potatoes.
Bed time snack:
- 1 small cup of cows or plant based milk.
- Handful of nuts.
- Small pot of natural or Greek yoghurt.
- Small handful of olives.
Summary
- Eat three regular meals every day.
- If hungry in between meals aim for a small snack containing carbohydrate between 10 – 15g (preferably low GI) or have a carb free snack,
- Avoid large meals – spread your carbohydrate portion as evenly as possible over the day.
- Balance your main meals with other nutrients coming from lean meat, fish, chicken or meat alternatives and plenty of salads/vegetables.
- Ensure good fluid intake, aim for 2 litres of sugar free fluid per day.
- Choose lower carbohydrate toast toppings such as peanut butter, cheese, marmite, and avocado instead of jam, marmalade, and honey.
- Exercise is important in pregnancy so aim for 30 mins of exercise daily. For instance, 15 – 20 minutes’ walk or longer after meals will help to control your blood glucose.
Other useful links
- Your guide to gestational diabetes | Free diabetes information
- Recipe finder - Enjoy Food | Diabetes UK
- Healthy eating in pregnancy - Start for Life - NHS
- Gestational diabetes | RCOG
© North Bristol NHS Trust. This edition published September 2025. Review due September 2028. NBT003601.
Support your local hospital charity

See the impact we make across our hospitals and how you can be a part of it.

