Welcome
North Bristol NHS Trust acknowledge that older people are an important and growing population in our community. We celebrate the fact that our population is living longer and commit to providing care and support for patients, carers, and their families. Our aspiration is to provide the best possible care and support for people living with Dementia and those who care for them in a holistic way.
Intro from Chief Nursing Officer

At North Bristol NHS Trust, we are committed to our focus of providing a high quality care for people living with dementia. We will deliver this through our dedicated workforce and amazing volunteers, developing their skills and knowledge through innovation and research.
A key aspiration of Challenge on Dementia 2020 (DoH 2015) is to create dementia friendly hospitals.
The National Dementia Action Alliance and Dementia Friendly Hospital Charter (NDAA 2019) contribute to improving the experience and outcomes for people with dementia in hospital care.
Within this strategy, there is recognition of the importance of taking a holistic person-centred approach when we deliver care. We recognise the need to support and engage with our patients who have dementia, their carers and family.
- Professor Steve Hams, Chief Nursing Officer
Our vision
Our vision is to put individuals at the centre of their own health and care. People will be inspired and supported to care for themselves more and to take an active role in how we provide care and treatment at NBT. Our services will become more joined up, informed by public decision making and where possible closer to or at home. Access to our leading-edge hospital and specialist services will be simplified and capable of best caring for the population we serve.
Our aspiration is to provide the best possible care and support for people living with dementia and those who care for them.
“Dementia is a long-term condition affecting memory, cognition, health and behaviour experienced by the person and their family/carers that can benefit from proactive planning, timely treatment, support and compassionate care”. Department of Health, Making a Difference in Dementia: Nursing Vision and Strategy (refreshed September 2016).
Our commitment
To empower people to have a more active role in their own care.
To ensure that people who use services and the professionals who provide care work together as partners.
Empowering people in their own care involves three core steps.
- Listening to our people about what matters to them
- Including patient voices in addressing areas of concern and give patients/carers an active role to participate in improving services.
- Working together to enable people to understand their health, condition, and treatment, enabling shared decision making.
We recognise there is more we can do to make this happen and need to start by sharing the journey of improvement that we have been on and giving patients and the public full confidence in the services that we provide.
We aspire to move towards understanding and involving the public more in decision making, using consistent and agreed co-design methodologies.
Our goals
- Our goal is to create a dementia friendly hospital in line with the ambitions of the Challenge on Dementia 2020 (DoH,2015). The National Dementia Action Alliance and Dementia Friendly Hospital Charter (NDAA 2019) supports improving the experience and outcomes for people with dementia in hospital care.
- In providing a dementia friendly hospital, we aim to work with the NICE guidance to support initiatives that will enhance this. (NICE, 2019).
- We will implement the principles related to reasonable adjustments to deliver the best quality experience of hospital care for people with dementia and their carers.
- North Bristol Trust fully supports and is committed to achieving this through exceptional healthcare personally delivered.
Introduction
A positive patient experience is about getting good treatment in a comfortable, caring and safe environment delivered in a reassuring way.
It is about having information to make choices to feel confident and feel in control. It is about being conversed with and listened to as an equal, treated with honesty, respect and dignity.
In NBT this is about communicating information to enable patients, family and carers to make informed choices. To feel supported is central to decision making and being in control. This requires an environment that enables candour and proactive listening.
NBT works to make enhancements to the environment for people with dementia.
NBT will work to promote social interactions and the use of art to create opportunities to ensure we provide the best experience for our patients and their families and carers.
NBT is committed to work in partnership with dementia charities and local providers. Within NBT we will grow and continue to support our dementia and carer champions.
Purpose of the Strategy
The launch of Challenge on Dementia 2020 (DoH 2015) is to create dementia friendly hospitals, and since the National Dementia Strategy in 2009 much has been achieved nationally and locally. However, dementia care continues to provide challenges to maintaining our achievements, toward implementing our objectives and planning for the future.
The aim of the strategy is to provide a clear overview and understanding of how staff and volunteers at NBT can support people with dementia when they are in our care.
This support could be as an inpatient, attending outpatients or day services or as family members or visitors to our hospital.
The Dementia Strategy sets out the objectives for exceptional healthcare personally delivered for people living with dementia recognising the vital role that family and carers provide.
Fundamental to NBT providing support is the relationship with the person living with dementia, the patient, the family/relative/carer and the healthcare professional.
The Carers Trust (2015) described this as the carer’s ‘Triangle of Care’.
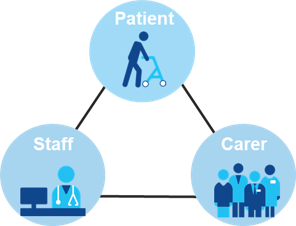
This promotes safe care and support through communication.
National and Local Picture
The number of people with dementia is increasing and this presents a significant and urgent challenge to health and social care, both in the numbers of people affected and the associated costs for their care.
There is no cure in sight and new, effective treatments are years away. More than one million people will be living with a form of dementia as of 2022, and this is set to rise significantly by 2025. As this number rises, so too does the number of families impacted by dementia, and the need for specialist advice and support( Dementia-UK- Strategy 2020-2025).
An estimated 25,000 people of Black, Asian and other Minority Ethnic (BAME) origins live with dementia in the UK – a number which is expected to increase sevenfold by 2051. Diagnosis is more likely to occur at an advanced stage of the illness, while there is a lower take-up of mainstream dementia services.
The most common complication leading to hospitalisation in the older population is due to delirium; occurring in 30% of patients attending emergency departments. It is significant that the incidence of delirium is higher in those with pre-existing cognitive impairment (dementia). It is therefore important to assess for and recognise delirium ‘an acute confusional state’ as it can be treated.
Ongoing research continues to look to prevent dementia and find ways of managing the quality of life for those living with the disease.
Modifying lifestyles may reduce the risks of developing dementia. (WHO 2019)
Dementia is a key priority for the NHS and can affect anyone whatever their gender, ethnic group or class.
Alzheimer's Society Key Facts (2021)
- 1 in 14 over 65 will develop dementia
- 850,000 people in UK are living with dementia
- Over 42,000 people under 65 years old are living with young onset dementia in the UK
- 1 in 6 over 80 year olds are affected by dementia
- An estimated 1,000,000 people will be living with dementia by 2025
- 25% of acute hospital beds are occupied by people living with dementia
In South Gloucestershire by 2025 an estimated 4,571 number of people ages 65+ will be living with dementia. There are approximately 2,062 people over the age of 65 living with dementia who have received a diagnosis (62.6%).
In Bristol there are an estimated 4,500 people living with the condition. Over the next 30 years, we expect that number to increase by a third.
In North Somerset there are over 3,100 people living with dementia.
Process of Delivery
North Bristol NHS Trust dementia team accepts referrals from all wards and departments providing assessments and ensuring appropriate ward based care for patients with dementia. The team delivers training to all staff members. They coordinate, advise and support a wider team of dementia and carer champions throughout the Trust.
NBT is fully committed to Johns Campaign; the right for carers to stay with patients with dementia, and the National Dementia Action Alliance (NDDA) dementia statements; that reflect the elements that people with dementia and their carers say are essential to their quality of life.
Ensuring our strategy is delivered
The Dementia Strategy will be delivered by the Patient & Carer Experience Group, Dementia Strategy Group, Dementia Champions, and Dementia Group.
The Patient & Carer Experience Group reports to the Patient and Carer Experience Committee.
The Dementia Strategy Group should consist of staff, Carer representatives and community partners, and reports to the Patient & Carer Experience Group. The Patient & Carer Experience Group meet quarterly and oversee the implementation and progression of the Dementia Strategy and Work Plan.
The terms of reference and membership of this group will be reviewed to ensure the team is able to support delivery of the strategy.
Engagement
We have engaged with patients when developing this strategy; to listen to and understand their views from their personal experiences of acute hospital care. Below are direct quotes that they shared with us:
"It is wise for the Doctors and Nurses to know you have Dementia and understand the history of the sort of problems you have had in the past.”
“It is also important they know you are a whole person… to put everything into context.”
“It is important that your carer in my case my wife is involved and knows what is going to happen.”
"Also important to all of us is that our carers know because we will forget."
“Importance of family and carers being involved and present when decisions are being made around plans because we (the patient) can forget.”
“We want referrals to dementia services ... not just ‘memory ‘ services because gives so much more.”
“I have very specific problems so it is very important to go to the same staff who know me. I feel secure and confident then. It doesn’t matter if it’s not the same ward but to know (the same Consultant) will come to see me”.
Our objectives
This is what NBT aims to provide for people living with dementia.
- Assessment
- Person-centred care
- Structured quality governance framework to provide safe exceptional care
- Skilled workforce
- Dementia friendly hospital/environments
- Care/family involvement in personalised care
- End of life care
- Research and innovation
Objective 1 - Assessment
- We will identify and assess people with a known dementia, cognitive impairment and /or delirium when they access any of our services.
- We will ensure all patients are screened for dementia / delirium / cognitive impairment. Where indicated we will offer a comprehensive assessment.
- Patients can be referred to the dementia team or other specialists teams such as the mental health liaison team.
- We will provide holistic care with input from Allied Health Professionals such as physiotherapists, occupational therapists, dietitians and speech and language therapists.
- Each patient will have a MUST score and an assessment regarding eating and drinking on admission.
- Discharge planning will be integral to the admission assessment process.
Objective 2 - Person-centred care
- We will provide excellent person-centred care in every interaction.
- We will ensure we have recorded each individual patient’s needs and plan care accordingly.
- We will continue to embed the implementation of personal life stories and information such as the ‘This is Me’ Alzheimer’s tool for patients with dementia and or delirium across all areas. Staff will be familiar with these using them to aid communication and to assist as a non pharmaceutical approach to providing care.
- A ‘My Life Story’ template that can be downloaded from the Dementia UK website.
- We will work closely with the patient’s relatives and carers the ‘Triangle of Care’ will be integral to their experience.
- We recognise it is essential to maintain links with families and carers.
- We will embrace use of technology to enhance care and evaluate the care we deliver.
- Learning from the Covid 19 pandemic, new approaches to using digital devices has provided a platform to access care and support carers. This will be built upon as we incorporate the benefits in the provision of our services going forward.
Objective 3 - Structured quality governance framework to provide safe exceptional care
- We will have outstanding leadership in dementia care by working through our Trust quality schedules.
- We will ensure that we learn from experience using quality information and a dashboard report to drive change / improvement.
- The Trust endorses a ‘Just’ and ‘Inclusive’ culture that seeks feedback and implements learning to improve and develop services.
- Each division has a patient experience and governance team that proactively participates in the wider governance structures of the Trust reporting to the Patient Safety Committee.
- The Dementia Strategy Group will work to a plan with accountability to the Patient and Carer Experience Group.
Objective 4 - Workforce: We will have an informed, confident and competent workforce
- We will ensure every member of staff has up to date training relevant to their role.
- We will ensure there are Dementia champions in every area (clinical and non clinical) and they have an exciting development programme.
- We will continue to recruit and develop Volunteers to support our patients and support meaningful activities.
- This will include exploring the Friendly Faces project, return of the Dementia Café, and working with Fresh Arts/Creative Companions
- We will plan and develop dementia training and support for volunteers who conduct roles such as befriending and mealtime companion.
- Training compliancy will be monitored and recorded and reported to the Dementia Strategy Group on a quarterly basis.
Objective 5 - Dementia Friendly Hospital/Environments
- We will ensure there is standardisation of ward and outpatient environments to ensure that all areas of the Trust are dementia friendly.
- We will use patient and carer feedback to improve areas of the hospital that have more people with dementia.
- We are committed to our participation in the PLACE (Patient Led Assessment of the Care Environment) to assess our compliance against the dementia friendly design recommendations included in the audit process since 2016.
- We will ensure that the environment is welcoming for relatives and carers.
- We will develop a sense of community for people with dementia, relatives and their carers.
- We will work in partnership with regard to the Learning Disability, Carers and Volunteers Strategy.
- We will co-produce audits or surveys for the best outcomes.
Objective 6 - Carer/family involvement in personalised care
- We will recognise the Carer and their role.
- We will maintain the hospital Carers Scheme and support John’s Campaign.
- We will develop care that is developed in the context of life, family, friends and community in which they live.
- We will work in partnership with community partners to facilitate safe transition from hospital and onwards care and support.
- We will work closely with services and providers to develop and innovate new ways of working. Ensuring we embrace the development and expansion of the use of digital and assistive technology.
Objective 7 - End of life care
- We will ensure that patients with dementia receive outstanding ‘end of life’ care within the ‘Purple Butterfly’ framework.
- We will ensure that advanced care planning and RESPECT (Recommended Summary Plan for Emergency and Treatment) is referred to or completed in a sensitive and timely way.
- We will develop personalised ‘end of life’ care for people living with dementia.
Objective 8 - Research and innovation
- We will work to be recognised as a dementia service that innovates, is involved in research and quality improvement.
- We will promote research and innovation in dementia care and support all professions to do so.
- We will through the ReMemBr (Research into Memory, the Brain and Dementia) Group engage with patients and carers to help us to design research studies for people with memory problems.
- ReMemBr link: https://www.nbt.nhs.uk/our-services/a-z-services/dementia-remembr-group/about-remembr-group
- We will use quality improvement methodology to drive change.
How we will measure and improve our dementia care
Through the Dementia Strategy Group we will develop a work plan related to the objectives and Trust values driven by:
Assessment
- A yearly audit of the Find Assess Investigate Refer and Inform (FAIRI) process related to the identification of patients with dementia/delirium.
- Review the National Institute for Health and Care Excellence (NICE) guidance around dementia and delirium.
- Register to participate in the National Audit of Dementia.
Person-centred
- Audit the completion of patients 'This is me’ documentation to support personalising care to individual needs.
Quality/Governance
- Report implement and monitor actions from audits carried out with regard to dementia care to and from the Dementia Strategy Group.
- Collaborate with the falls academy, end of life group and carers group.
- Work with future developments and implementation of the National Audit for Dementia.
- Implement a dementia dashboard that will report quarterly to the Dementia Strategy Group.
Workforce
- Develop and maintain the dementia champions.
- Ensure training is accessible to all staff groups within the trust.
- The Dementia Team to celebrate local or individual quality projects that have been undertaken by Dementia Champions at an Annual Dementia Conference.
Environment
- Complete the annual Patient-Led Assessments of the Care Environment (PLACE).
Carer/family involvement
- Coproduce and work in partnerships with carers feedback and views.
- Continue to network and work in partnership with local community groups and the wider strategy groups of Bristol North Somerset and South Gloucester (BNSSG).
End of Life Care
- Audit the completion of RESPECT forms and Advanced Care Planning for a sample of patients to inform the outcomes of the Ageing Well initiatives and ‘end of life’ care for patients with dementia.
Research and Innovation
- Inform and communicate through the Dementia Team and Dementia Strategy Group new developments relating to the care of patients with dementia.
This strategy will require us to continue to build on the achievements and the commitment and energy of staff, volunteers, partner organisations and patient and carer representatives to ensure delivery.
Acknowledgements
- John's Campaign
- Alzheimer's Society
- Carers Support Centre, Bristol & South Gloucestershire
- Young Dementia Network, hosted by Dementia UK
- Dementia Action Alliance (DAA)
