What is botulinum toxin-A? What is it for?
Botulinum toxin-A (Botox) is a prescription medicine that can be injected into the bladder muscle. In our department, it is used to treat overactive bladder (OAB).
OAB is a condition that can cause a sudden strong feeling of needing to pass urine (urgency) which can sometimes be associated with leakage (urgency incontinence). It may also result in patients needing to pass urine more frequently. This treatment does not help people with stress urinary incontinence (leakage when you exercise, sneeze or strain).
Botox is currently the only licensed formulation of Botulinum toxin-A to be used in the bladder. It is used for treating urodynamically diagnosed detrusor over activity and/or urgency incontinence. Patients diagnosed with this can receive a dose of 100 units into the bladder. Patients with neurogenic detrusor over activity, for example patients with complex neurological conditions such as multiple sclerosis can receive a dose of 200 units. Very rarely do people need 300 units.
Each patient’s case is discussed in the lower urinary tract symptoms (LUTS) multidisciplinary team meeting (MDT) and every patient is assigned the appropriate treatment and dose based on their symptoms and diagnosis.
How effective is the procedure in helping with overactive bladder symptoms?
- Botox injections are effective in about 7 in 10 patients (70%), meaning that the urgency and/or urgency incontinence are either significantly better or improved.
- The effects of the injections can last for around 6 to 9 months.
- When your symptoms start to return, you can have further injections.
- There is no limit to how many times you can have your Botox repeated, but you cannot have a repeat within 4 months of each injection.
- Most people find that having repeat injections works well over many years.
- There are no obvious long-term negative effects of having repeated Botox injections into the bladder.
What does this procedure involve?
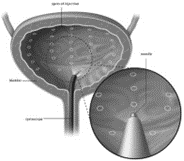
The procedure involves passing a small telescope (cystoscope) into your bladder, through your urethra (water pipe), and giving several injections of Botox into your bladder wall with a needle passed through the cystoscope. Botox paralyses the muscle of the bladder wall and prevents your bladder muscle from contracting and giving you the urgency symptoms.
What are the benefits?
The aim of the injections is to reduce urinary symptoms such as frequency (passing urine often), urgency and urgency incontinence. It is unlikely that you will see immediate improvement in symptoms and it may take between 2 to 6 weeks to gain maximum benefit.
The effects of the injections usually last between 6 and 9 months, although this can be variable. Repeat injections will be required each time the effects wear off. This can be offered no more than every 4 months due to the risk of build-up of the toxin in your body.
What are the alternatives?
You are being offered invasive treatment on the basis that you have not had a good response to conservative and medical therapy for your symptoms.
Overactive bladder may be a lifelong condition and we currently have no cure. All treatments are aimed at helping you cope with the symptoms (see ‘overactive bladder syndrome’ leaflet NBT002734). We recommend that all patients try conservative and medical treatments initially before having invasive procedures. Alternative, conservative measures include:
- Incontinence pads – you may choose not to have any invasive procedures and use incontinence pads to contain your urinary leakage.
- Conservative measures – including weight loss, improving fluid intake and reducing caffeine.
- Bladder training – learning techniques to hold on and override your urgency to pass urine.
- Medicines – these may help if conservative treatment does not work.
Botox injections are usually only tried if the above treatments are not effective. Other treatments that can be used instead of Botox injections include:
- Posterior tibial nerve stimulation (PTNS) – electrical stimulation of the tibial nerve via your ankle can be used, but is not available here in Bristol and not widely available on the NHS as it is not highly recommended by NICE (National Institute for Health and Clinical Excellence).
- Sacral neuromodulation – a device (battery and wire) is implanted in your lower back that sends electrical signals that modulates/stimulates the bladder nerves – a ‘pacemaker’ to the bladder. This is offered here in Bristol and we could make an appointment for you to discuss this in more detail (see NBT003133 leaflet).
- Enterocystoplasty – a major operation that enlarges your bladder using a piece of bowel.
- Urinary diversion (ursotomy) – creating a stoma using a piece of bowel to divert the urine into a bag.
Why might we not give you Botox?
- Botox is not given to patients who have signs or symptoms of urinary tract infection, in individuals with known hypersensitivity to any botulinum toxin preparation or to any of the components in the formulation.
- It is also contraindicated in patients who cannot perform clean and intermittent self-catheterisation or accept a long-term indwelling catheter if they go into urinary retention.
- Botox must be used with caution in patients with neuromuscular disorders, such as myasthenia gravis, as it may affect the muscles involved in breathing.
Prior to Botox treatment
This treatment improves the bladder symptoms by essentially paralysing the bladder. This can also mean that the bladder does not empty properly and you may need to self-catheterise. Therefore, prior to your appointment for Botox treatment, if you don’t already know how to self-catheterise, you will be seen by one of the specialist nurses and taught how to perform clean intermittent self-catheterisation (CISC).
This involves you learning how to pass a small plastic tube into your bladder in order to drain urine. This tube is thrown away once the bladder is drained and the procedure may be repeated several (usually 1-4) times a day. If you are unable to perform self-catheterisation, the alternative would be using a long term urethral or suprapubic catheter, and this can be discussed further with the specialist nurses. CISC may be required until the effect of the Botox wears off.
You will be invited to an appointment either in theatres or the outpatient’s clinic where the procedure can be performed under general, or local, anaesthetic. You will be telephoned by one of the admin team and they will ask you some very important questions and it is important to be honest in your answers or you may be cancelled on the day of the procedure.
On the phone, you will be asked questions such as:
- Do you have a catheter or can you perform CISC?
- Do you have recurrent urinary tract infections? If you suffer with recurrent urinary infections, or in the days prior to the procedure you have symptoms of a urinary tract infection, then you should attend your GP surgery to have your urine checked for an infection and a sample of urine sent to the lab to be analysed by Microscopy, Culture and Sensitivity (MC&S). If you do have an infection, please complete your treatment before coming in for the Botox injections. If your urine test taken in the hospital prior to the procedure is negative for infection and you feel well, we will go ahead with the procedure. If you have an untreated urinary infection on the day of the procedure, it will be cancelled.
- Have you had any other Botox injections anywhere else in the body in the last 3 months? If you had botulinum toxin of any formulation anywhere else in the body within the last 3 months, you will not be able to have it in your bladder unless they are 3 months apart.
- Do you have any mobility issues? We can prepare the appropriate equipment to help you.
- Are you on any medications that thin the blood? These medications may include Anticoagulants such as Clopidogrel, Warfarin, Rivaroxaban, Apixaban, Dabigatran, Edoxaban and a dose of Asprin higher than 75mg. If you are on such medications, then a preoperative assessment will need to be arranged to stop the medication safely prior to the procedure.
What happens on the day of the procedure?
- If your procedure is being completed in outpatients under local anaesthesia then you may eat and drink as normal and take your usual medications.
- You will be invited to attend Gate 36 in the urology department.
- On arrival to the department, the nursing team will ask you for a urine specimen. It is important that you do this in the department so it is fresh. The procedure will not be able to go ahead if you are not able to produce a urine sample to rule out infection. If you do have an infection, the procedure will be abandoned and you will be rebooked with appropriate antibiotics beforehand.
If your procedure is being completed in theatres under local or general anaesthesia
- You will be invited to attend the theatres department.
- You may be asked not to eat and drink and not to take your medication. If you have any questions regarding this, please contact the department beforehand.
- On arrival to the department, the nursing team will ask you for a urine specimen. It is important that you do this in the department so it is fresh. The procedure will not be able to go ahead if we don’t have a sample to rule out a urine infection. If you do have an infection, the procedure will be abandoned and you will be rebooked with appropriate antibiotics beforehand.
- Wherever you have the procedure, you will be seen by the specialist nurse or doctor who will go through the plans of your procedure and ask you questions regarding your medications, allergies, previous Botox injection, and how you empty your bladder.
- Once you have answered the questions and had the opportunity to ask your own questions, you will be asked to sign a consent form which clearly states the potential risks and side effects of the procedure you are having.
What are the potential risks and side effects?
- Urinary tract infection (15%-20%) - see your GP if you have symptoms of burning/stinging when passing urine as you may require a course of antibiotics. We will give you oral antibiotics to go home with for 5 days.
- Blood in the urine (8%-20%) - this is usually minor and settles down without any treatment. If you however continue to bleed then you would need to seek medical advice and you may need a surgical procedure under general anaesthetic to stop the bleeding.
- Urinary retention (7-10%) – some patients will have difficulty emptying their bladder fully after Botox. This is helped by beginning intermittent self-catheterisation which is taught prior to the procedure, for as long as is needed. If you are unable to do self-catheterisation then you would be offered a suprapubic catheter (small permanent indwelling tube through the lower part of the ‘tummy’) to help drain the urine until the Botox wears off. We would not recommend having a permanent indwelling catheter going through the urethra for a long time due to the damage it causes to the soft tissues in the genitals.
- Bladder Pain (5%) – very occasionally, some patients develop a pain in the bladder following injections. This pain is usually controlled with simple painkillers such as paracetamol and typically resolves quickly following the injections. If this continues please attend your GP surgery.
- Generalised muscle weakness (less than 3%) – this is very rare. Some patients have reported weakness in muscles of the arms and the legs at other hospitals across the world. They have been reported to be mild and usually do not require a stay in hospital. The condition resolves with time although it can take several months. There is no specific treatment for this if it occurs.
- Allergic reaction – this is rare, however, get emergency medical help if you have any of these signs of an allergic reaction: hives, difficulty breathing, feeling like you might pass out, or swelling of your face, lips, tongue, or throat.
- Temporary ‘flu-like’ symptoms are experienced rarely – some patients who have had Botox have reported these symptoms for a week or two after the injections.
What takes place during the procedure?
If you are happy to go ahead you will be asked to undress in privacy. You will be provided with a hospital gown to wear to cover yourself; this will avoid any water from the cystoscopy coming in contact with your clothes. If you wish to stay in your own clothing on the upper half of your body then please let the doctor or nurse know. If you wish to keep your socks on then please bring a spare pair with you in case they get wet. If you feel cold in the hospital gown, then please let one of the staff members know and they will help cover you with blankets.
In the urology department there is usually a specialist nurse or doctor and at least one other staff member in the room available to help you. There may also be visitors to the unit as we are a national and international training centre. Please let your doctor know if you do not wish to have any visitors in the room during your procedure. This is your right.
If the procedure is completed in theatres there will be a specialist nurse or doctor and a number of theatre staff to look after you and assist with the procedure. An anaesthetist will also be there if you have a general anaesthesia.
You will be asked to lie down on a couch. The specialist will then clean your genitalia with warm cleaning fluid and cover you with sterile drapes. This is important to protect you from infection after the procedure. A small amount of lubricating jelly is injected into the urethra, lubricating the area so you feel less discomfort. This may sting a little. A small telescope is then passed into your bladder. Your bladder is filled with salt-water (normal saline) through the telescope which may make you feel like you need to go to the toilet to pass urine. Sometimes there is leakage of water around the telescope but this is normal and the doctors and nurses expect it to happen. The nurse or doctor then passes a small needle down the telescope and injects between 10 and 20 injections of Botox into your bladder. The telescope and needle are then removed. You can then go and empty your bladder as normal.
The procedure may be uncomfortable but should not be painful. As the Botox is being injected, it can sting for a few seconds. If the procedure becomes uncomfortable you can ask the doctor or nurse to stop. The actual injection process may take about 10 to 15 minutes but expect to be in the department between one and two hours. In theatres however, you may expect to be there for some hours.
What happens after the procedure?
If this is your first time, you will receive a telephone follow up from one of our specialist nurses at around 6 weeks to check up on your progress.
You may also be seen in the outpatient department 6-9 months after you have received your Botox if you request this.
Following this, you will simply need to contact us once the Botox wears off to book your next session.
You may also be approached regarding involvement in research and taking part in trials. If you are involved in a trial, your follow up plan may vary according to the trial protocol.
What is my risk of hospital acquired infections?
Your risk of getting an infection in hospital is approximately 8 in 100 (8%): this includes getting MRSA and Clostridium Difficile bowel infection. This figure is higher if you are in a ‘high-risk’ group of patients.
Driving after surgery
It is your responsibility to make sure that you are fit to drive after any surgical procedure. You only need to contact the DVLA if your ability to drive is likely to be affected for more than 3 months. If it is, you should check with your insurance company before driving again.
What should I do with this information?
Thank you for taking the time to read this information sheet.
Please make note of the link for your own records. You may be asked to sign a form saying you understand the information.
If you do decide to proceed with the scheduled procedure, you will be asked to sign a separate consent form which will be filed in your hospital notes and you will, in addition, be provided with a copy of the form if you wish.
References
Kuo HC, Liao CH, Chung SD. Adverse events of intravesical botulinum toxin a injections for idiopathic detrusor overactivity: Risk factors and influence on treatment outcome. Eur Urol. 2010;58:919–26
Orasanu B, Mahajan ST. The use of botulinum toxin for the treatment of overactive bladder syndrome. Indian Journal of Urology : IJU : Journal of the Urological Society of India. 2013;29(1):2-11. doi:10.4103/0970- 1591.109975.
Idiopathic overactive bladder syndrome: botulinum toxin A | Advice | NICE
© North Bristol NHS Trust. This edition published April 2023. Review due April 2026. NBT003281
