North Bristol Trust is one of two Major Trauma Centres in the South West of England treating approximately 1,200 severely injured patients each year. Whilst mortality has reduced since Major Trauma Centres were introduced in 2012, post discharge and rehabilitation concerns remain the most common issues identified.
Before Quality Trauma Discharge
The discharge process had been focused solely on the patient leaving hospital rather than as an opportunity to educate and facilitate enhanced recovery. High levels of anxiety, uncertainty about provision of care post discharge and confusion about medication were frequently described at follow up as well as unscheduled healthcare attendances. Over 70% of the patients surveyed in the pre-intervention phase had visited their GP at least once in the first thirty days. Frequently these patients reported that this was because they wanted information about their injuries and about ongoing treatment: GPs are often unable to provide this.
QTD is now an integral part of the service we provide to our patients and their families. The intervention is delivered in the main by the Major Trauma Practitioners working at the Major Trauma Centre and is now being offered to both those patients discharging home and transferring to a local inpatient unit within the Major Trauma Network. Currently approximately 20-30 patients per month receive the QTD ‘package’: decisions to offer this are based on discharge plans and clinical need.
No additional staffing has been required for implementation, but the drive to offer QTD has necessitated re-evaluation and streamlining of the Major Trauma Practitioner or key worker role. There is now evident focus on the needs of each individual patient throughout their pathway beyond emergent and acute care and the preparation for this starts during early contacts turning the ‘discharge’ into a process rather than a one-off event.
Electronic Portal – Patients Know Best (PKB)
During the development phase, the project team decided that the QTD care plans should be housed in an electronic patient-held record. Currently we are using Patients Know Best (PKB).
Through a web-based application, the PKB solution puts the patient in control of their health records and, by granting access to specific care providers, creates a single instance of the relevant care record that is available wherever the patient receives treatment. It is securely hosted within the NHS N3 network.
Allowing patients to securely access their own health information and providing them with the ability to connect health professionals and carers together in one ‘place’ enables them to take control of aspects of their own healthcare.
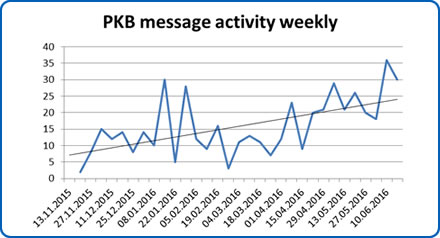
In the first year of using the electronic portal as our method of delivery for the AHCP we identified a consistent increase in the number of online messages that the team were receiving. It is clear that patients are using the messaging service to communicate concerns and problems to the team.
Although the numbers weren’t formally recorded, the trauma practitioners agreed that there was a comparable reduction in the number of telephone calls made to the existing patient helpline over the same time period. This allows the team to interact with their patients and resolve their queries more efficiently. The written messages also provide both a reliable record of advice for the patient to refer back to and also a clinical audit trail. This pattern has remained consistent over the subsequent eighteen months of the QTD initiative.
QTD is now viewed by the Severn Major Trauma team as an integral part of the service we provide to our patients and their families. There is no doubt that the opportunity prior to discharge for a patient and their carers and relatives to sit down and speak with an expert professional is exceptionally valuable. People have described the experience as ‘reassuring’ and as ‘answering questions I didn’t know I had’. Our data suggests that this empowers people to be more confident in managing their care and seeking help appropriately.
Feedback
Reduces anxiety about being “forgotten” within the hospital system as major trauma provide a point of contact.
Gives you an excellent overview of the patient, their injuries and treatments.
Allows the patient and their family time to ask questions and voice concerns.
Builds rapport so gives the patient an opportunity to be truthful or open up.
Helps patients and families feel at ease about being discharged from hospital.
Allows for clarification of follow up plans and appointments.
Having someone there to speak to for longer than 5 minutes.
