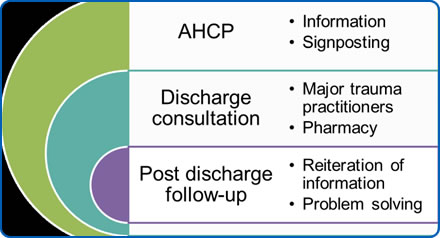
The Quality Patient Discharge intervention consists of three simple, interlinked elements:
Download sample resources:
My Way Forward document
A personalised information pack detailing patient-specific information about diagnosis, medication, outpatient follow-up and signposting the patient which way to turn with any questions or concerns. This is to reinforce information which they have already been given during their admission, not to give new information, and should act to empower patients and carers. This document can be issued as a paper copy, however, by utilising an electronic platform accessible to patients and ‘invited’ others the plan becomes a more dynamic, responsive resource for patient, carers and clinicians. Download

Discharge consultation
An Individualised ‘discharge counselling’ session for the patient and family or carers with an appropriately trained keyworker around twenty-four hours prior to planned discharge. A pharmacist will also see the patient at this time and give education around medication. This one-to-one time should give opportunities for any questions or concerns to be addressed prior to discharge and will be based around the ‘after hospital care plan’.
Tailoring the discharge package to the patient based on the consultation means that all of the information given, follow up arrangements, contact details and prescribing information are held by the patient or carers in one format. Download
Two week call

Feedback
I always think of questions just before I go to bed. I can’t call someone at that time… If I send a message straight away, I know that I’ve taken action and someone will pick it up in the morning. Then my brain will switch off and I can go to sleep.
Feedback
As far as I recall no-one actually told me while I was in hospital, so extraordinary as it may seem I actually had no idea of the extent or severity of my condition until sometime after I arrived home. It was only reading the notes from my admission on this website that I fully realised what had happened.
