This page has information for patients about pelvic floor exercises for women.
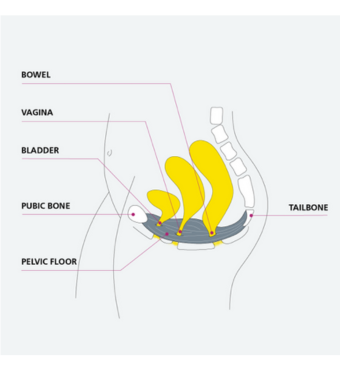
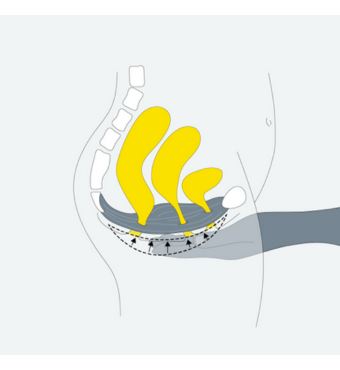
Where are the pelvic floor muscles?
Your pelvic floor muscles are a group of muscles that attach from the pubic bone at the front of your pelvis to the coccyx and sacrum at the back of your pelvis.
What are the functions of your pelvic floor muscles?
- To maintain bladder and bowel continence
- To hold the bladder, bowel and uterus in place to prevent pelvic organ prolapse
- To enhance sensation during sexual intercourse and your ability to orgasm
- To help with birth
- To stabilise the pelvis
Why do pelvic floor exercises?
- 1 in 3 women have urinary incontinence
- 1 in 10 women have faecal incontinence
- 1 in 2 women have pelvic organ prolapse
Doing your pelvic floor exercises can help reduce the risk of developing urinary incontinence, faecal incontinence and pelvic organ prolapse.
Factors that can weaken your pelvic floor muscles and increase the risk of developing some of the symptoms
- Pregnancy.
- Vaginal birth.
- High BMI (Body Mass Index).
- Chronic constipation.
- Chronic cough.
- Menopause.
- Other health conditions e.g. uncontrolled diabetes, Multiple Sclerosis (MS), a stroke.
Therefore it is important to avoid constipation, maintain a healthy BMI and get a cough treated.
Pelvic floor exercises are important for all women, particularly if you:
- Leak when coughing, sneezing, laughing or physical exertion.
- Have difficulty controlling wind.
- Leak before reaching the toilet.
- Are pregnant or have recently had a baby.
- Are menopausal or post-menopausal.
Finding the pelvic floor muscles
Sit comfortably on a firm chair with your knees slightly apart or lie down.
- Tighten your back passage (anus) – as if you are stopping yourself passing wind. Do not squeeze your buttocks or leg muscles. Do not hold your breath, continue to breathe normally.
- Tighten your vagina/front passage – as if you are trying to stop the flow of urine. Try to feel the muscles lifting upwards and forwards towards the pubic bone.
- Feel the muscles working together, then relax.
- Tighten the pelvic floor muscles as above and hold this. How many seconds can you hold? Aim for 5 seconds – when you let go, can you feel the muscles relax? If not, you have held too long – try again with a shorter hold. Some women may be able to hold for only 1-2 seconds and others as many as 8-10 seconds. It is important to discover your hold time.
Pelvic floor exercises
Do these exercises sitting or lying down.
Exercise 1 - slow pull-ups
Take a breath in, on the breath out tighten the pelvic floor muscles slowly. Continue to tighten for your length of hold, relax, and feel the muscle let go. Rest for 5 seconds. Repeat this 5 times. As it gets easier, gradually increase length of hold and number of repetitions, aiming for 10 seconds.
Exercise 2 - fast pull-ups
Tighten the pelvic floor muscles quickly. Let go straight away. Repeat this 10 times – approximately 1 contraction per second.
Pelvic floor exercise routine
Do exercise 1 and 2 at each session. As soon as you can, increase to 10 slow and 10 fast pull-ups. Aim to repeat each session at least 3 times each day, so in total you will be doing 30 slow and 30 fast a day.
As your muscles get stronger you may progress to doing the exercises in standing.
You may not see immediate improvement, but do not give up. You need to continue this routine for at least 4-6 months. As the muscles get stronger you will be able to increase your hold time and number of repetitions at each session.
Do not practice stopping the flow of urine midstream as this may interfere with the normal process of emptying your bladder.
The Knack
Try to get in the habit of tightening your pelvic floor muscles before you cough, sneeze or lift anything.
To help ensure you do your exercises daily try to link it to an everyday activity, for example, when brushing your teeth or waiting at traffic lights. You can also download an app called Squeezy which is recommended by the NHS. It will send you reminders to do the exercises and you can personalise the programme to suit you.
Additional tips
- Being constipated or overweight can strain the pelvic floor muscles so eat a balanced diet including fruit and vegetables.
- Drink between 6 and 8 cups of fluid a day.
- Avoid caffeinated, fizzy and alcoholic drinks if you suffer from urgency or frequency (the need to pass urine more often than normal) as these may worsen the urgency and frequency.
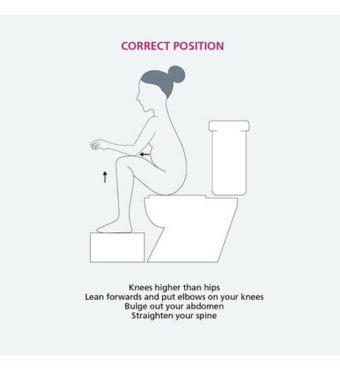
- You may also want to try sitting in the correct toilet position to help with opening your bowels, the picture below demonstrates this. (This is sitting on the toilet with your feet on a foot stool, knees higher than hips, lean forwards and put your elbows on your knees, bulge out your abdomen, and straighten your spine).
Specialist referral
If you have difficulty identifying your pelvic floor muscles and have symptoms, you can self-refer to Pelvic Health Physiotherapy via the My Joint Health Hub website.
If you are unable to self-refer, please speak to your healthcare provider and they can refer you to your local Pelvic Health Physiotherapy provider on your behalf.
Key points
- Continue the pelvic floor exercises several times per day for the rest of your life in order to keep these muscles fit and healthy. If symptoms return, increase the amount of exercises you do each day.
- When you are contracting your pelvic floor muscles it is only an internal contraction so there should be no movement from the outside.
- If your problem is ‘urgency’ (needing to get to the toilet quickly), tighten your pelvic floor muscles when you get the desire to empty your bladder; wait until the desire passes before moving.
Resources and references
Useful resources
Squeezy app - available on iPhone and Android.
References
Laycock, J and Haslam, J (2008) Therapeutic management of incontinence and pelvic pain. Springer Verlag. (2nd ed) NICE Clinical Guideline [NG123] (2019) Urinary incontinence and pelvic organ prolapse in women: management. Available at: https://www.nice.org.uk/guidance/ng123
© North Bristol NHS Trust. This edition published July 2023. Review due July 2026. NBT002529.
