Information for patients who have had a skin graft.
About skin grafts
What is a skin graft?
A skin graft is the transfer of healthy skin from one part of the body to replace the burn wound. The skin graft must be taken from your own skin as skin donated from friends, family will be rejected by your body.
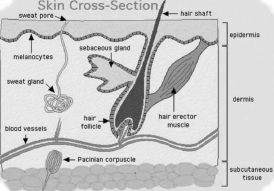
The skin is a very important and provides a protective barrier to the organs in the body; it prevents infection and water loss. When the skin is damaged by a burn or scald the protection is lost. If the burn is deeper than the top layer of skin a skin graft may be required, the burns team will explain and discuss your surgical and wound management options.
A skin graft is necessary when the cells needed to repair the skin have been lost or damaged and new cells are needed. This is due to the burn wound extending deeper into the skin dermal layers and cells that would normally heal the burn wound have been destroyed. Without a skin graft the risk of infection is high, you may incur a delayed wound healing time or the burn wound may not heal at all.
‘Image taken from EnchantedLearning.com with permission’
How is the skin graft taken?
This is a surgical procedure, which will require a general anaesthetic. The surgeon will take a thin shaving of healthy skin and put it on the cleaned burn wound. This new wound is called the ‘donor site’ and will have a dressing on it.
How does the skin graft stay in place?
The skin graft may be stapled, stitched or glued, depending on the size and depth of the graft and the site of the wound, most grafts are glued. The graft will then have a dressing over it for protection. These techniques depend on the patient, the size of the skin graft and the area where it is applied or on the consultant’s instructions. If the graft is on or near a joint, a splint may be used to reduce movement to protect the graft.
How long do these wounds take to heal?
The healing time will depend on the size and depth of the wound. The aim is to get the wound healed in about two weeks, but healing may take longer. Infection can slow down healing. Smoking can also affect healing. It is advisable to try to stop smoking.
Are there any risks?
The risks will be explained by the surgeon when they ask you to sign the consent form for the operation. The risks include bleeding (in some cases a blood transfusion may be required, this will be discussed with you) infection and partial or complete loss of graft. Re-grafting may be required if the wounds are over a large area or some or all the graft is lost.
Please ask your doctor or nurse if you would like further information about any of these points and poor nutrition.
After a skin graft
What dressings will be used?
Both the donor site and skin grafts will be covered by dressings (unless they are on the face). The dressings might be different each time they are changed but this will be explained by your nurse. The type of dressings may also change as the wounds heal. Please ask the nurse if you have any questions about the dressings used.
When I can I start walking after a skin graft?
It can depend on where it is. If it is anywhere other than your leg(s), you can start walking as soon as you feel up to it. If it is on one or both of your legs, then we encourage you to stay on bed rest for several days or until the skin graft is secure enough for walking on. The nursing staff will advise you when you can start to walk. You may be referred to a physiotherapist to help with this.
What can help the wounds heal?
It is important that the care instructions given by the surgeons and nurses are followed, to give the graft a good chance of healing. A healthy balanced diet that includes plenty of protein is important. Protein foods include: milk, cheese, yoghurts, eggs, meat, fish. Smoking and passive smoking slows down the healing by reducing the amount of oxygen reaching the skin.
Will I need to keep it dressed when I go home?
Yes. In the early days a protective dressing will be necessary. This may be changed in our adult burns clinic and if you are unable to attend this will be changed by a district nurse or by your GP practice if you can attend there. You will have to return to the hospital for follow up appointments to see the doctors.
What will my grafted skin look like?
With any skin graft, scar formation is inevitable, but the appearance of your graft will change considerably over the weeks and months to follow, so its initial appearance should not cause alarm. This can be of a meshed netted pattern appearance or small fenestrated lines depending on the depth of skin graft taken from the donor site. It can take up to two years for a scar to ‘mature’, usually leaving a pale, soft and supple scar.
Once the graft is healed you will be referred to the scar management team as you may be at risk of developing scarring. This can appear as raised, red, firm, itchy scarring which may develop for about three months after you have healed. The scar management service will closely monitor this and provide appropriate treatment if required.
Small areas of wound breakdown and blisters are common on the newly healed skin as it is thinner and more sensitive. This may occur due to irritation from clothing or accidental bumps and bruises. If this happens these can be protected with small dressings to prevent further damage and help healing.
How do I care for the skin graft once it is healed?
Skin grafts have fewer oil and sweat glands, so tend to become dry. When the graft can be left exposed and is completely healed, it should be kept clean by gently washing it as normal. Avoid very hot water and never use highly perfumed soaps, creams or bubble baths. After bathing gently pat the grafts dry and then massage the area with non-perfumed moisturising cream or simple emollients as least twice a day to keep the area supple. This is only usually kept up for six months. You will be given advice on this prior to discharge and by the scar management team.
Will I need to wear any support when I go home?
You may be advised to wear Tubigrip (an elastic stocking) as part of your rehabilitation plan by the scar management team.
Is there any other advice I should know about caring for my skin graft?
It is very important that both the skin graft and donor sites are protected from the sun as it is new thinner skin without the normal skin protection. It is very important that for the next two years/summers that you apply high factor sun protection (both form UVA and UVB) or use total sun block cream and wear sun protective clothing over these areas, as new skin will burn and blister very quickly.
Sun burn to graft and donor sites may worsen appearance of these areas. If it becomes tanned this can be a permanent tan that can be blotchy.
Donor sites
What is a donor site?
A donor site is the area left when a piece of skin graft has been taken to cover a defect on another part of the body. There are various parts from where the skin can be taken, such as the thigh, upper arm, or even the buttocks.
How long will it take for the donor site to heal?
It usually takes around ten to fourteen days. The dressing applied in theatre at the time of your operation will stay in place for that period and should be kept clean and dry. A donor site is like a bad graze, so the dressing protects the raw surface and allows it to heal. It also soaks up any fluid that naturally seeps from the wound. This can sometimes cause a strange odour, but that is normal.
Will the dressing need to be changed before the ten to fourteen day period?
There are times when donor area dressings do need to be changed, such as if the dressing becomes very loose or if there is an excessive loss of fluid through the dressing. This can be done by the hospital nurse if you are still a patient or by your local practice nurse if you have been discharged home.
If the dressing gets loose wet or dirty reapply the outer layers/ contact the practice nurse but do not touch or interfere with the wound. Ensure your wound is kept covered until it is fully healed.
Will I get any pain from the donor site?
Some people experience more pain than others, usually within the first 48 hours. Regular painkillers, such as paracetamol can be taken.
Who will remove the dressing when it is due to be taken off?
On discharge you will be followed up in our adult burns clinic if you still have burns dressings in place. If you are unable to attend our acute burns clinic then the ward staff will arrange either the district nurse or practice nurse to change your dressings. We maintain close links with the community team.
The dressing usually loosens itself as the wound heals. Otherwise it can be soaked off in the bath or shower. If the area is fully healed and dry, then it can be left exposed, and you can massage in moisturising cream or simple emollients, twice a day.
Do not apply it to raw areas as this can cause blistering.
Do I have to be careful about the clothing I wear?
Try not to wear articles of clothing that may make you itch or may be too tight. But if you find that some clothes do rub, a protective dry dressing should be worn.
Will my donor site look like normal skin when it’s healed?
You can expect your donor site to change colour. At first it can look bright red, but over several months it will become slightly darker (depending on your skin type) paler or rougher than normal skin i.e. donor sites tend to always be different, albeit very slightly.
Eventually it will blend in, but it may end up slightly paler than your surrounding skin.
Advice should be taken from your doctor about lifting, stretching and returning to work.
Important advice
Sun screen advice:
It is very important that both the graft and donor sites are protected from the sun as it is new thinner skin without the normal skin protection. It is very important that you apply high factor sun protection cream (for both UVA and UVB) and wears protective clothing over the areas, as the new skin will burn very quickly and blister. If it becomes tanned this can be a permanent tan that can be blotchy. It is important to protect all newly healed areas from sun damage for at least two years.
Pain and itching:
You may still require medicines after discharge from the hospital to help with pain and itching. Medication will be discussed with you prior to your discharge home.
Itching can be a problem for some people. Regular creaming and massage helps. Wearing loose clothes made from natural materials can also help. If your itching will not settle and becomes a problem please speak to the doctor or nurse at the hospital. There are medicines that can help.
Scar management:
Following skin grafts there will be scarring. Once the wounds have healed you will be referred to the scar management team who will treat the scars to produce the best outcome.
Treatments may include:
Creaming and massage, silicone creams and gels and pressure garments. These will be discussed with you when the wounds are healed. If you are worried about the scarring and you have not been seen by the scar management team, please discuss your concerns at your next follow up appointment with any member of the burns team.
Please contact the Adult Burns help line: 0117 414 3100 / 0117 414 3102.
Help from the psychologist
If you are finding it difficult to come to terms with the treatment plan or with the scars then help is available. Please speak to your nurse or surgeon at the hospital who may be able to help with this. It may be that you would benefit from seeing a clinical psychologist.
The Adult Burns Team are here to help, please ask us any questions you may have about the information in this leaflet or any other issue.
References, support, and further information
References
Management of Grafts and Donor Sites
British Journal of Nursing (1998) 7: 6,324-334
Management of Skin Grafts and Donor Sites
Nursing Times (2007) vol 103 No 43, 52-53
Patient support
Useful patient support web sites are listed below. If you think it would be helpful and if you wish to meet a burns survivor then please do discuss this option with a member of the burns team.
Adult Burns Unit
Burns | North Bristol NHS Trust (nbt.nhs.uk)
Adult Burn Support UK
Adult Burn Support UK – Information, support and advice about burns in the UK
A support resource for adult burn survivors in the UK.
Email: info@adultburnsupportuk.org
Funded by Dan’s Fund for Burns national charity.
Dan’s Fund for Burns
Dans Fund For Burns – Giving burn survivors the help they need
Dan’s Fund for Burns is a national charity offering practical help to burn survivors in the UK. The charity identifies those most in need of help and provides it in a swift and practical way.
Changing Faces
Changing Faces | Visible Difference & Disfigurement Charity
Changing Faces is a charity for people and families who are living with conditions, marks, or scars that affect their appearance.
Online Health Talk
Healthtalk
Information about skin grafts and pressure garments
Katie Piper Foundation
www.katiepiperfoundation.org.uk
The Katie Piper Foundation aims to:
- Progress intensive rehabilitation and scar management for burns survivors.
- Provide information on, and access to non-surgical treatments for burns and scars.
- Campaign for consistent clinical care.
- Develop a support network for people living with burns/scars.
- Help people with burns/scars reconnect with their lives and their communities.
The Lee Spark NF Foundation
Help & Support for Dealing with Necrotising Fasciitis (nfsuk.org.uk)
To help those whose lives have been affected by necrotising fasciitis and other severe streptococcal infections.
Outlook
Outlook | North Bristol NHS Trust (nbt.nhs.uk)
Psychological support for people with appearance concerns.
The Fire Fighters Charity Helpline
Monday-Friday, 09:00 - 17:00.
The Fire Fighters Charity has a wealth of experience in providing helpline services on a wide range of issues, directing to other relevant benefits that might be available to you, or organisations that may be able to provide assistance.
Skin camouflage
Bristol Laser Centre | North Bristol NHS Trust (nbt.nhs.uk)
Acid Survivors Trust International (ASTI)
www.acidviolence.org
A registered charity based in the UK operating as a centre of excellence supporting and working hand in hand with Acid Survivors Foundations (ASFs) in Bangladesh, Cambodia, Uganda and Pakistan.
Burns Unit contact numbers
Adult Burns 24 hour helpline
Adult Burns Clinic (Monday-Saturday)
Burns Clinical Psychology appointments through Acute Burns Clinic Coordinator
(Monday-Friday)
Scar Management Service/Occupational Therapy (Monday-Friday)
(Monday-Friday)
07525 618 421
SMC@nbt.nhs.uk
Physiotherapy (Monday-Friday)
Outlook: psychological support for people with appearance concerns
(Monday-Thursday)
Oral Surgery (face masks)
(Monday-Friday)
© North Bristol NHS Trust. This edition published February 2024. Review due due February 2027. NBT002776.
