What is gynaecomastia (male breast)?
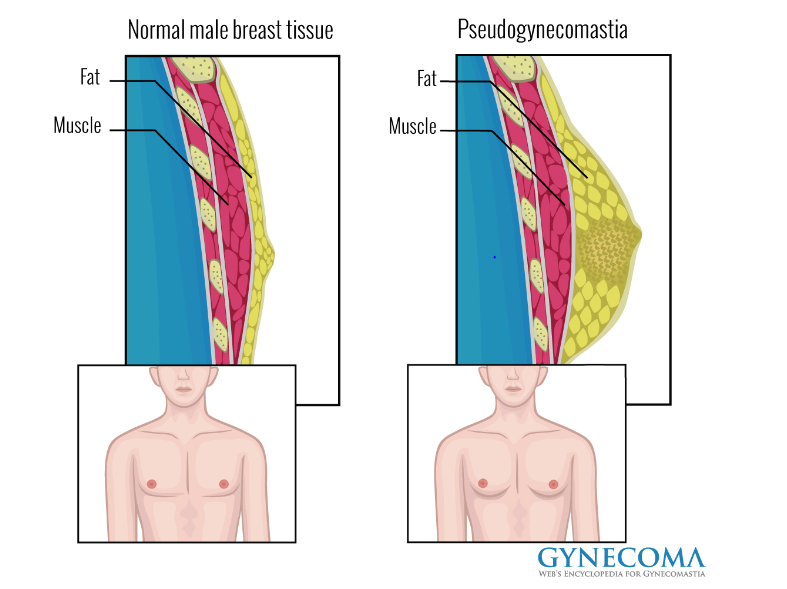
Gynecomastia can occur in babies, teen boys, and older men, it can be referred to as ‘man boobs’. This condition is the overdevelopment of the male breast (see diagram 1).
Diagram 1: shows both normal and enlarged male breast tissue
What causes gynaecomastia?
Hormone imbalance
All men produce both male and female hormones. The female hormone is called oestrogen and the male hormone is called testosterone. If the balance of hormones in the body changes for example producing too much oestrogen or too little testosterone, this can cause a man’s breasts to grow. The amount of excess tissue growth will vary from a small amount of extra tissue around the nipples to enlarge breasts (see diagram 2). This can affect one or both breasts. The breast tissue can be tender or painful, but this isn’t always the case. The cause of the imbalance of hormones may be unknown.
Diagram 2:
Being overweight
A common reason for gynaecomastia is being very overweight. The reason for this is that the excess weight may increases the production of oestrogen being made by the body which can cause breast tissue to develop. However, some growth in breast tissue might not be due to extra body fat from being overweight. Therefore losing weight or doing more exercise may not improve the condition.
New-born baby boys
Gynaecomastia can affect new-born baby boys, because oestrogen passes through the placenta from the mother to the baby. This is temporary and will disappear a few weeks after the baby is born.
Puberty
During puberty, boys’ hormone levels vary. If the level of testosterone drops, oestrogen can cause breast tissue to grow.
Many teenage boys have some degree of breast enlargement. Gynaecomastia at puberty usually clears up as boys get older and their hormone levels become stable.
Older age
As men get older, they produce less testosterone. Older men also tend to have more body fat, and this can cause more oestrogen to be produced. These changes in hormone levels can lead to excess breast tissue growth.
Other causes
In rare cases, gynaecomastia can be caused by:
- side effects of medication, such as anti-ulcer drugs or medication for heart disease
- recreational drugs, such as cannabis or anabolic steroids
- drinking too much alcohol
- kidney failure or liver disease
- Klinefelter’s syndrome (a rare genetic disorder)
- lumps or infection in the testicles
How is gynaecomastia diagnosed?
At the clinic you’ll have a breast examination. In some case, you may need to have other tests so that a definite diagnosis can be made. These can include:
- a mammogram (breast x-ray) and/or ultrasound scan (which creates a picture of the breast using high-frequency sound waves)
- a fine needle aspiration (FNA) or core biopsy of breast tissue. An FNA uses a fine needle and syringe to take a sample of breast cells for analysis under a microscope. A core biopsy uses a larger needle to remove a sample of breast tissue rather than cells and is performed under local anaesthetic.
- because gynaecomastia can be a symptom of other conditions, such as hyperthyroidism (overactive thyroid gland), the consultant may also want to examine your testicles, neck and abdomen. They may also ask you to have further tests, for example a blood test.
What can be done to correct gynaecomastia?
Non-surgical options
Medication
Your doctor may decide that you need to be treated with hormonal drugs. The different hormonal drugs used to treat gynaecomastia are Danazol, Tamoxifen and very occasionally Aromatase inhibitors. Although these hormonal treatments are not licensed for use with gynaecomastia, they have been shown to be useful in treating it. Your doctor will need to follow you up regularly if you are prescribed any of these drugs. There are no guidelines on which treatment should be considered first. However, there is usually a preference to use tamoxifen and danazol. While you’re taking these drugs you may experience side effects, so they’re only suitable for use following a thorough discussion of their benefits and risks.
Psychological Therapy Team - Outlook
Outlook is part of the Plastic Surgery Service which provides psychological support for people with appearance concerns. Our consultant clinical psychologist and specialist counsellor have experienced in providing you with coping skills regarding self-consciousness related to appearance. An appointment lasts for about one hour, which gives you time to talk things through regarding your breast asymmetry. This therapy can be really useful. If you feel that you may benefit from this therapy we can refer you to this service or your GP can.
Surgical options
Gynaecomastia may be treated either by using liposuction which sucks out the fatty tissue or by surgically removing the firmer layer of tissue, or a combination of two methods. Surgeons aim to reduce the breast size to normal contours, to eliminate painful tissue and to restore the patient’s chest to an acceptable cosmetic shape.
Please be aware of the following:
- Gynaecomastia surgery is considered a procedure of low clinical priority and therefore not routinely funded under the NHS. Hence, your GP will need to apply for NHS funding for this operation to be carried out.
- Patients must have completed puberty. Therefore surgery is not normally commissioned for people below the age of 19 years.
- Gynaecomastia has been present for more than two years.
- If you are considering gynaecomastia surgery you will need to keep your BMI under < 27 for one year prior to your surgery. Your weight and height will be taken and recorded in your medical notes as evidenced of your calculated BMI. Failure to achieve this goal will mean that you will not be considered fit for your operation.
How are decisions made on NHS funding?
At present the Clinical Commissioning Groups (CCGs) decide what will and will not be funded within the NHS and the majority of Gynaecomastia surgery is considered low priority and many applications for funding are denied. You may find that one or several appeals need to be made on your behalf by your GP to your local CCG for consideration of surgery, but this still may not result in funding being granted.
All funding requests should be made by your GP.
When considering funding, the CCG may take account of the following:
- If there is natural absence of breast tissue unilaterally (one breast) or bilaterally (both breasts).
- That you are aged 18 or over - to ensure you have reached the end of puberty and stopped growing.
- It is recommended that the BMI (body mass index) is within the healthy range.
- You must be a non-smoker.
Following your consultation with the plastic surgeon a letter will be sent to your GP which will detail the degree of gynaecomastia. This may be used as supporting evidence when your GP applies for CCG funding.
The treatment options discussed in this leaflet are subject to CCG funding approval.
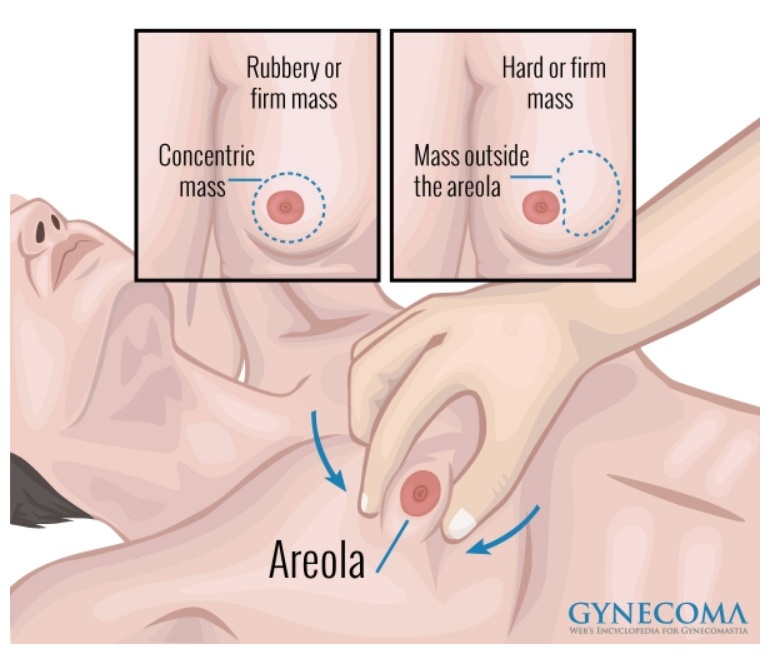
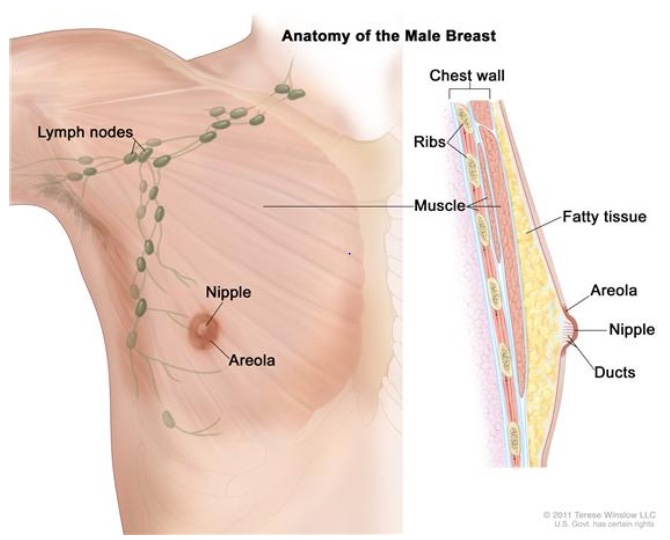
Before we discuss treatment options it is important to know the names of the different parts of the breast as this section will be discussing the chest muscle which is called the pectoralis or pectoral muscle, nipple and areola. Diagram 3 shows you a picture of the breast which is labelled to indicate the position of the areola, nipple and pectoral muscle.
Diagram 3:
What does the operation involve?
The operation takes between one to one and a half hours is performed under general anaesthetic and involves being admitted to hospital as a day case or overnight stay. This will depend on which procedure you are having as you may have a combination of both these procedures.
- Liposuction – The surgeon will insert a thin hollow cannula (tube) into the chest area. The surgeon moves the cannula around under the skin to suck out the fat cells. The small puncture wound will then be closed with dissolvable stitches and/or covered with a small dressing.
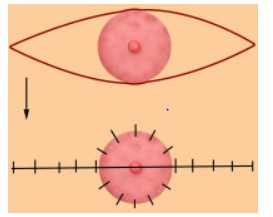
- Direct excision – The surgeon will make a semi-circular incision (cut) around the areola (nipple) edge and remove the excess layer of tissue. The incision is closed with dissolvable stitches and covered with a small dressing.
Diagram 4:

Are there any risks?
Complications with this operation are rare, but can occur.
- The most common complication of direct excision is a haematoma – a collection of blood in the space where the fat has been removed.
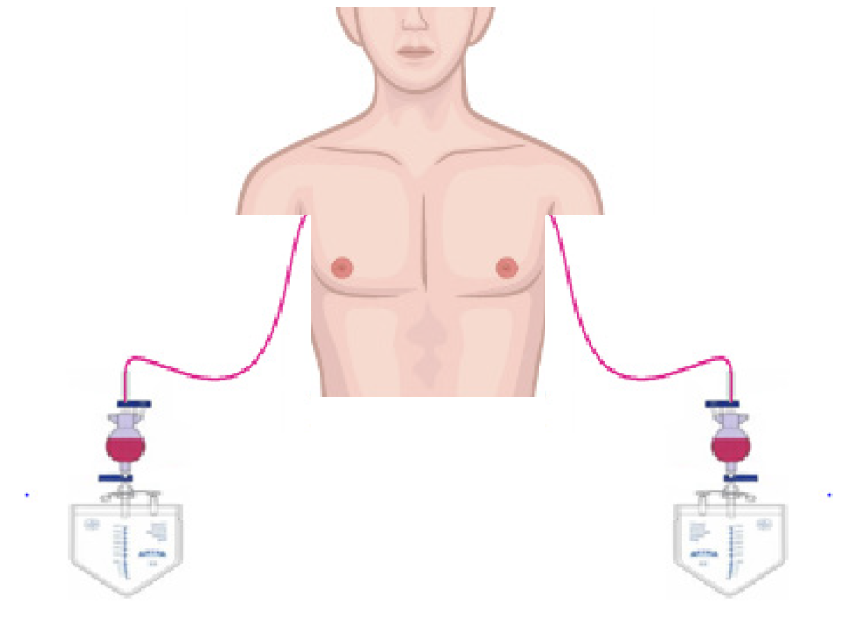
- If the haematoma is small, it will be left for the body to absorb it naturally over a period of days or weeks. If it is large, this may require a second operation to drain the old blood, but this will not affect the final outcome of the operation. See diagram 5.
- The other main complication is infection, which is true of all surgery, but this can be minimised by careful hygiene after the operation.
- Nipple necrosis: this is where the tissue to the nipple doesn’t receive enough blood, thus some or all of the tissue can die
- Nipple flattening, inversion or loss of sensation.
What happens after the operation?
You will return to the ward after the operation to allow them to recover from the anaesthetic. You can start eating and drinking as normal once they feel like it. Most patients stay overnight after the operation and go home the following day.
The chest area will be quite swollen after the operation – and for a while afterwards – so it is important not to judge the results of the surgery for several months. You will need to wear a pressure garment for the first six weeks after the operation. This will help reduce swelling and make the area more comfortable.
What happens when I return to the ward?
Once you return to the ward the nurses will monitor your urine output and record your blood pressure, pulse and temperature. The nurse will check your nipples for colour, warmth and sensation. Dressings will be checked to ensure that they are clean and dry. The nurse will also check that your drains are draining.
Diagram 5
Will I have any pain after the operation?
You may experience some discomfort but we will give you painkillers to control any pain you may have. Please note this may vary from one person to another depending upon the individual’s pain threshold.
What happens the next day after the operation?
The nurse will check your dressings the next day according to the doctor’s instructions. If you have drains they will be removed providing the blood loss is between 30-50ml. It is important to bring a Firm Control Vest into hospital, and this should be worn day and night for six weeks. See diagram 6. The nurse will help fit the vest to ensure that it is fits correctly.
Diagram 6: Firm Control Vest


Going home
You will probably need pain relief for a few days after the operation as the area will be quite sore. The nurses will explain how much medication to give and how to take the medication.
What if I smoke?
Smoking can reduce the blood flow to surgical sites. Studies have shown that nicotine and other substances that are found in cigarettes can be harmful to your heart, lungs, and your skin. Smoking can have an adverse effect on the healing of all surgical wounds. The same applies for the use of nicotine replacement therapy as, although this will reduce the craving for a cigarette, the nicotine will also reduce the ability of the blood to carry enough oxygen to the tissues.
For this reason we advise that you do not use nicotine replacement therapies and should stop smoking completely. The plastic surgeon will not be considered if you smoker. Hence, If you are an active smoker we will advise you to go to your GP for support or visit the Smokefree National website: http://www.nhs.uk/smokefree on how to get help in stopping smoking.
What if I drink alcohol?
During your consultation you will be asked how much alcohol you drink. Therefore, it is important that you keep to the recommend alcohol units guidelines set by the department of health which is 2-3 units per day for women. If you drink more that the recommended allowance this will mean that your operation will not take place until your alcohol units are in keeping with NHS guidelines. This is to prevent any complications occurring following your anaesthetic/operation as you will experience symptoms of alcohol withdrawal this will affect wound healing and recovery.
For practical information on alcohol, visit NHS choices change for life.
What if I have a high Body Mass Index (BMI)
At your consultation with your plastic surgeon you will be weighed and your height measured this will calculate your BMI.
If your BMI is greater than 27 this will mean that your operation will not take place until you have lost weight.
If this is the case your GP can help support you to lose weight, by providing you with a weight loss program. For practical weight loss information visit, NHS choices change for life.
Once you have achieved your goal of a BMI of 27 you will need to maintain this for a year prior to having your operation.
Category and BMI (kg/m2)
- Very severely underweight - less than 15
- Severely underweight - from 15.0 to 16.0
- Underweight - from 16.0 to 18.5
- Normal (healthy weight) - from 18.5 to 25
- Overweight - from 25 to 30
- Obese Class I (moderately obese) - from 30 to 35
- Obese Class II (severely obese) - from 35 to 40
- Obese Class III (very severely obese) - over 40
NHS website for weight loss information http://www.nhs.uk/tools/pages/healthyweightcalculator.aspx
Contact information
If you have any further questions or need advice regarding the information in this leaflet please contact one of the Breast Reconstruction Nurse Specialists.
Breast Reconstruction Nurse Practitioner
Caroline Oates
Breast Reconstruction Nurse
Caroline Lewis
Tel: 0117 414 8700 or 0117 950 5050 bleep 1698 (answer machine available)
Email: caroline.oates@nbt.nhs.uk
caroline.lewis@nbt.nhs.uk
Secretary for Ms Jackson & Ms Patel
Andrea Thompson
Tel: 0117 414 7626
Email: andrea.thompson@nbt.nhs.uk
Secretary for Mr Wilson
Wendy Rodman
Tel: 0117 414 7633
Email: wendy.rodman@nbt.nhs.uk
Psychological Therapy Team Outlook
Telephone: 0117 414 4888
E-mail: Outlook.dsu@nbt.nhs.uk
British Association of Plastic Reconstructive and Aesthetic Surgeons (BAPRAS)
www.bapras.org.uk
If you or the individual you are caring for need support reading this leaflet please ask a member of staff for advice.
How to contact us:
Brunel building
Southmead Hospital
Westbury-on-trym
Bristol
BS10 5NB
0117 414 8700
© North Bristol NHS Trust. This edition published July 2021. Review due July 2023. NBT003412
