This page aims to help you understand frozen shoulder. It is not a substitute for professional medical care and should be used along with treatment from your healthcare professionals. Everyone's situation is individual. You may be given specific advice that is not included in this page.
The shoulder
Your shoulder joint is a ball and socket joint (like a mortar and pestle). The ball at the top of your arm bone (the humerus) fits into the socket (the glenoid) and this is the part of the shoulder that moves. The socket is part of the shoulder blade (the scapula).
The joint is surrounded by soft tissue forming the capsule - imagine it like a wrapper surrounding a chocolate. The shoulder gives a large range of movement which allows us to do our daily activities.
Frozen shoulder (adhesive capsulitis)
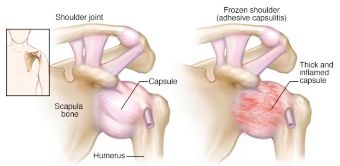
Frozen shoulder, also known as adhesive capsulitis, is where the shoulder becomes painful and stiff. It is often not obvious why this pain and stiffness has started. Normally, the soft tissue around the shoulder joint (capsule) is stretchy and elastic. This allows the joint to move. In a frozen shoulder, the capsule has become inflamed and thickened (fibrous). This leads to the pain and stiffness.
How common is it?
Frozen shoulder affects about 2-5% of people and commonly occurs in people aged 40-70. Between 6-17% of people with frozen shoulder, go on to develop it in the other shoulder, within five years of their first episode.
Symptoms
- Pain that limits your full range of movement. Pain often interferes with sleep.
- Joint stiffness, which limits your range of movement and daily activities.
Symptoms might become gradually worse over a number of months or years. See the stages below for more details.
These symptoms can make your everyday tasks frustrating and challenging. For example, you will likely have difficulty getting your hand behind your back for a long period of time. This movement is one of the last movements to return when you are in recovery from frozen shoulder.
Stages
The symptoms can vary over time in severity and overlap. To help guide treatment we may classify your symptoms into 2 phases:
- Painful predominant phase - where pain is the main problem and may interfere with your sleep.
- Stiffness predominant phase - where the stiffness or lack of movement is the main problem.
Recovery rates vary and usually last 2-3 years. However up to 40% of people can have symptoms for more than 3 years.
Causes
It is not clear what causes frozen shoulder, but there are many factors which put someone at higher risk. These include:
- Diabetes (type 1 or 2): 10-20% of people with diabetes develop frozen shoulder.
- Other conditions: hypothyroidism and hyperthyroidism, cardiac disease, Parkinson’s.
- Previous shoulder injury or surgery.
- Dupuytren’s contracture.
- Previous frozen shoulder.
Treatments
Most people with frozen shoulder will eventually get better. However, there are treatment options that can reduce pain and improve the movement in your shoulder.
The type of treatment will depend on your specific situation. It will also depend on whether the pain or stiffness limits you more.
- During the painful stage, the emphasis will be on reducing your pain.
- During the stiffness stage, the emphasis will be on improving your range of motion.
Next we will discuss hydrodistension injection which is one of the treatment options for stiffness.
Hydrodistension injection
This injection uses X-ray or ultrasound to guide it into the shoulder joint. Local anaesthetic and a steroid is injected into the shoulder. Extra fluid (sterile saline) is also injected into the frozen shoulder joint to try to stretch the capsule. This aims to give pain relief and improve your shoulder movement. It feels the same as a normal injection but with the added benefit of stretching the capsule.
At North Bristol NHS Trust, we do this in the Radiology (X-ray) department as an outpatient appointment. You won’t need to go to theatre or have sedation. This is a good option for people who have had their symptoms for six months or longer and has shown faster improvements in pain and movement than other injections.
On the day of the procedure
- Take your normal pain relief one hour before the injection
- Inform the Radiology department if you:
- Are pregnant.
- Have diabetes.
- Feel unwell.
- Have an infection, cold, or persistent cough.
- Have any allergies.
- Are taking any of the following medications:
- Antibiotics, aspirin, warfarin or clopidogrel or any other tablet to thin the blood (some of these may have to be stopped some days before).
The procedure
You will lie on your back, with your arm (frozen shoulder) out to the side. The skin will be sterilised and the local anaesthetic will be given. This will numb the area.
Using an X-ray, a fine needle will then be inserted into the joint. A small amount of X-ray dye (iodine contrast) will be injected into the joint to make sure we have found the best position for the needle. Once in the best position, 15-40mls of a mixture containing more local anaesthetic, steroid, and fluid (saline) will be injected into the shoulder.
You may feel some pressure and pushing. If you do feel discomfort please tell the radiologist.
Risks
General risks:
- Allergic reaction to the steroid, which may be life threatening (anaphylaxis).
- Bleeding.
- Infection: if the injection area becomes red, hot, and swollen and you feel unwell, seek help immediately.
For steroid injections
- Skin thinning, dimpling, and change of skin colour at the site of the injection.
- Facial flushing for a few days.
- Occasionally symptoms may get worse for couple of days. You can take your painkillers if you need to.
This list does not cover everything. If there are further risks or complications your consultant will tell you these before the injection.
What happens after the injection?
Pain and discomfort
You may feel some moderate pain and discomfort following the injection. This typically lasts less than 30 minutes.
You will stay in the department for 15-30 minutes after the injection and then you will be discharged home.
A numb sensation in the shoulder is normal from the anaesthetic and this often lasts around eight hours. You should not drive the day of your injection; your insurance may not cover you. It is your responsibility to call your insurance company about driving after the injection.
If you have diabetes
Closely monitor your blood sugars after the procedure for 48 hours. Your insulin requirement may increase due to the steroid.
You will need to be monitor your glucose levels for 1 month after the injection. If you have any issues managing your diabetes, speak with your diabetes specialist nurse or see your GP.
Will my symptoms come back?
Research shows that 7.8% of people’s frozen shoulder may come back and may need another injection.
Physiotherapy
This section will take you through a progressive activity programme. This is important to maximise the benefit you get from the injection (Robinson et al., 2017).
- The day of the injection (day 0) - do the exercises 2 times a day while your shoulder is still feeling numb. Once your shoulder is no longer numb, stop the exercises.
- Day 1 - no exercises (this allows the steroid to work).
- Day 2 - no exercises.
- Day 3 - start the exercises again. Do them every day from this point.
Exercises
Pendulum - do this 10 times clockwise, 10 times anticlockwise. Let your arm hang, relaxed straight down. Gently swing your arm as if drawing a circle. Change direction.

Using a broom for external rotation. Do this 10 times. Sit with both elbows at right angles. Hold a stick with both hands. Push the stick to rotate the arm outwards as far as comfortable. Keep your elbows by the side of your body as shown.

Climbing up the wall with fingers and supporting the affected arm. Do this 10 times. Stand facing a wall. ‘Walk’ your fingers up the wall as high as comfortable. ‘Walk’ your fingers back down again.

Using the kitchen table and walking away stretching the arms and shoulders. Do this 10 times. Standing. Hold onto a table, slowly walk backwards, moving your body away from your hands.

Using a towel to pull up the arm to the mid back (bra strap). Do this 10 times. Stand or sit. With one arm, bring a towel/belt over your shoulder, behind your back. Hold onto the towel with the affected arm. Gently pull up, bringing the lower arm up. your back as able. Hold 5 – 10 seconds.

Follow-up
The clinician who referred you for the injection should arrange a further review 6-12 weeks after the injection. Please contact them if you do not already have an appointment.
If you have already seen a physiotherapist at North Bristol NHS Trust and are on a Patient Initiated Follow-Up (PIFU) appointment please ring 0117 414 3131 to book a review with your physiotherapist.
Information on adhesive capsulitis
© North Bristol NHS Trust. This edition published October 2025. Review due October 2028. NBT003791
