You have been advised by your hospital doctor to have an investigation known as ERCP (Endoscopic Retrograde Cholangio-pancreatography).
What is an ERCP?
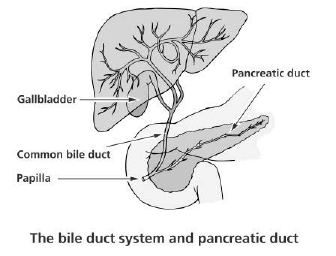
This is a medical examination performed to diagnose and treat disorders of the bile duct, gallbladder, pancreas and liver.
Why is an ERCP performed?
The most common reasons to do an ERCP are jaundice (yellowing of the skin or eyes) or abnormal liver tests or if a scan (ultrasound or CT scan) shows a blockage of the bile of pancreatic ducts. Blockages can be caused by stones, narrowing of the bile ducts and growths or cancers of the pancreas and bile ducts.
During an ERCP, stents (small plastic or metal tubes) can be inserted into the bile ducts to allow bile to drain into the intestine. If indicated a therapeutic procedure can then be undertaken. This may involve the removal of gallstones by cutting a larger opening in the bile duct (sphincterotomy) allowing the stones to fall out. An ERCP can give more information about the pancreas and bile ducts and brushings and biopsies (specimens of cells) can be taken from the bile ducts or the pancreas for analysis.
What happens before the procedure?
- You will have attended pre-assessment clinic or completed a telephone assessment to perform standard checks e.g. blood tests, MRSA test and medication checks.
- You can continue taking your normal medication. However, if you are on any medication which thins the blood (e.g. aspirin, clopidogrel, warfarin, rivaroxaban, dabigatran, apixaban) we ask you to call the interventional radiology department using the number on your appointment letter as we may need to adjust your medication before undergoing this procedure.
On the day of the procedure
- You should not eat or drink anything from 6 hours before your procedure so that the upper intestine is clear of food and liquid.
- You will arrive at the Imaging Department (Gate 19) and be accompanied into our day case area.
- Please inform us if you have any allergies.
- Please inform us if you think there is a chance you may be pregnant.
- A doctor specialising in the digestive system will discuss the procedure with you. You will have an opportunity to ask questions about the procedure and your treatment. If you choose to have the procedure you will need to sign a consent form.
- You will be asked to change into a hospital gown and a small plastic tube (cannnula) may be put into a vein in your arm to allow us to administer medications or intravenous fluids during the procedure.
- Once all the checks have been performed and consent signed, you will be taken to the angiography suite on the trolley. There will be a doctor, nurses and radiographer with you throughout the procedure.
During the procedure
- A nurse will attach monitors to record your pulse and oxygen level, as well as monitor your blood pressure and heart rhythm.
- You will be given a local anaesthetic throat spray to help numb the throat.
- You will need to lie on your left side and a plastic mouth guard will be placed in your mouth. This allows the telescope to pass through your mouth.
- We will give you oxygen through a small soft tube placed into your nostril.
- You will be given an injection of intravenous sedation and painkiller through the cannula in your hand. These medicines will relax you and may make you drowsy but will not necessarily put you to sleep.
- A nurse will stand by your head and monitor you for the whole procedure.
- Once you are drowsy the endoscope will be passed through your mouth, down your gullet into the stomach and then into the top part of the small intestine (duodenum).
- The doctor will insert a fine wire through the scope into the bile duct and inject a dye which shows up on x-ray.
- If stones need to be removed from the bile or pancreatic ducts, a small cut (sphincterotomy) may be made in the lower end of the bile duct to allow a fine tube to pass through. This also allows a small basket or balloon to be inserted to grasp a stone or stones.
- Specimens may be taken from the bile ducts using a small brush or forceps, and a plastic or metal tube (stent) may be inserted to help with the drainage of bile or pancreatic juice.
An ERCP usually lasts between 30 and 60 minutes depending on its complexity.
Taking your medications:
It would be helpful to bring a list of your current medications.
It is advisable to take your regular medications with a small amount of water no less than two hours before your test i.e. blood pressure tablets. Except:
- Diabetic Tablets or Insulin: Please contact your diabetic nurse or GP in advance of your procedure to discuss the appropriate measures. If necessary your GP surgery can seek further specialist advice from the hospital diabetes Centre.
- Anticoagulant and Anti-platelet drugs: eg. Warfarin, Coumadin, Clopidogrel, Rivaroxaban, Dipyridamole, Apixaban, Dabigatran.
Please make sure that you are told when to stop this medication by the doctor who referred you for this procedure. The level of the blood test (INR) must be <1.3 on the day of your procedure. If necessary your GP surgery can seek further specialist advice from the hospital haematology department.
What to expect after the procedure
- You will be taken back to the radiology day case unit, so that nursing staff may monitor you closely.
- If you are in pain tell the nursing staff so you can be given appropriate painkillers.
- You will be required to stay in our day case unit for 6 hours.
- Please make arrangements for someone to collect you from the hospital and take you home by car, as we advise not to use public transport. You are not permitted to drive for 24 hours post procedure and we would like someone to stay with you at home in the first 24 hours. Please inform the department if this is not possible, as we will need to identify alternative arrangements.
Furthermore, you should avoid the following activities after the procedure:
- Driving.
- Operating machinery.
- Drinking alcohol.
- Signing any legally binding documents.
- Carrying out any activities involving cooking, heights, bending, exercises.
- Caring for young children (sole responsibility).
Please check with your travel insurance if you wish to travel within 4 weeks of your procedure.
If you start to feel unwell or feverish, or develop severe abdominal pain, you must contact your GP or the local GP Emergency Service as soon as possible, it may be necessary to re-admit you to hospital.
You may resume a normal diet when able to do so.
Side effects and possible complications of ERCP
After the procedure your throat may feel sore for up to twenty-four hours. The indication for this test will have been determined by previous tests, such as an ultrasound scan, and considered to be the safest way to help you. However, an ERCP is not risk free.
You should be aware of the following possible complications:
- Failure to gain access to the bile duct due to differences in anatomy which occurs in 1/10 cases and may require a repeat or alternative procedure at a later date.
- Inflammation of the pancreas (pancreatitis) is due to irritation caused by contrast and occurs in 4/100 cases. This causes abdominal pain and is usually self-limiting. However, in 1/100 cases it can require a prolonged stay in hospital.
- Sometimes a cut is made in the intestine (sphincterotomy) which allows the release of displaced gall-stones. In 1/140 cases bleeding occurs which is usually controlled during the ERCP. Perforation of the intestine can occur in 1/1000 cases. Both situations can require open surgical correction.
- Death is a very rare outcome after ERCP. It occurs following severe complications of the type outlined above. The national mortality figure following ERCP is one in 3000 cases lead to complications that can result in death.
References
Bennet, J.R (1981). Therapeutic Endoscopy. Chapman and Hall.
Doctor Online (1999). ERCP www.doctoronline.nhs.uk
Gelton, P. and Williams, C (1997). Practical Gastrointestinal Endoscopy. Blackwell Science Ltd.
Hadley, A and Martin, D. Having an ERCP: A guide to the test.
Keymed.
“Having an ERCP” Guy’s and St Thomas’ NHS Foundation Trust 2018. Leaflet number: 2559/VER4 Accessed 24/07/2019.
© North Bristol NHS Trust. This edition published January 2024. Review due January 2027. NBT002079
Imaging Department Contact Centre
If you are unable to attend your appointment please let us know as soon as possible. You can also contact the Imaging Department Contact Centre if you wish to change or discuss your appointment.
Telephone: 0117 414 8989
Support your local hospital charity

See the impact we make across our hospitals and how you can be a part of it.
