This page will provide you with information about longer term feeding tubes. The page will tell you what to expect before, during and after your operation.
A member of the medical team, your dietitian or your speech and language therapist can answer any further questions you may have.
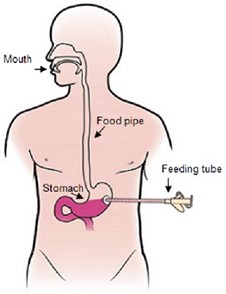
What is a feeding tube?
A feeding tube is a small tube that passes through the skin into your stomach. This allows special liquid feed, water and medicines to be passed into the stomach. It can help to meet your dietary needs.
The three different operations used in North Bristol Trust are:
- Percutaneous Endoscopic Gastrostomy (PEG) – uses a flexible camera (endoscope) that passes into your stomach.
- Per-oral Image Guided Gastrostomy (PIGG) – the tube is placed using x-ray.
- Radiologically Inserted Gastrostomy (RIG) – the tube is placed using x-ray.
The most common tube is the PEG. You may have a RIG or PIGG tube if you cannot have sedation or if the camera cannot access your stomach. We will discuss with you which type is best.
Why do I need a feeding tube?
There are many reasons why you may need a feeding tube. We will discuss this fully with you. You may consider a feeding tube when:
- You are losing weight.
- You cannot eat or drink enough.
- Eating and drinking leads to choking or discomfort.
- Your breathing function is reduced or you get chest infections.
- It takes a long time to eat and it is no longer enjoyable for you.
- You have been getting nutrition through a tube in your nose for many weeks (nasogastric tube (NG)).
- The feeding tube in your nose keeps coming out.
- It is unsafe for you to eat or drink.
Sometimes feeding tubes are placed if you have problems with swallowing.
Will a feeding tube stop me eating and drinking?
Not always, but this will be discussed with your doctor or speech and language therapist.
The tube itself will not affect your ability to eat and drink. Some patients decide to still eat small amounts for pleasure. Some use the tube to provide extra nutrition on top of what they eat and drink.
What are my other choices if I decide against having one?
If you decide not to have a feeding tube, it is unlikely that there are any other ways to meet your dietary needs. You should discuss your choices with your doctor and dietitian.
If you decide against tube feeding you will be supported in this decision. Please make sure you know the risks you may be taking.
How do I prepare for a feeding tube?
All types of feeding tube are placed in hospital.
If you are not already on a ward:
- A few days before the operation you may have a blood test and a swab taken by the GP.
- You may be asked to stop taking certain blood thinning medications for a few days before the operation. You may receive a phone call with more information before the operation.
- You will need to come in on the day of the operation.
If you are an inpatient:
- The ward team will advise you about stopping any blood thinning medications. They will also complete blood tests.
Before the operation:
- You will be asked to have no nutrition (food) for at least six hours before the operation. You will also be asked to have no fluids for two hours before the operation. You may be given medication through a drip.
- The doctor will examine you, explain the operation and ask you to sign the consent form.
You will likely stay in hospital for at least a night for monitoring.
Are there any risks?
Most people will not have any serious issues from their tube placement. However, the risks of a complication increase with age. Your risk of having issues is also increased if you have from heart, chest, or other medical problems, such as diabetes, or are overweight, or smoke.
Major complications occur in around 3 in 100 people and include:
- Breathing problems.
- Heart complications.
- Peritonitis (swelling in stomach wall).
- Bleeding.
- Bowel perforation (accidental tear in your gut).
- Wound infection.
- Fistula formation (two organs connect).
- Leaking around the tube.
- Tube blockage.
- Buried bumper (stomach grows over part of the tube).
- Over granulation (excess skin grows on the tube).
- Infection.
There is a low mortality rate. To minimise complications, we will choose the technique that is safest for you.
How is the tube placed?
If you are having a PEG
This is done in the Endoscopy Department. You will be given a local anaesthetic to your stomach, some throat spray, and light sedation (to make you feel relaxed). An endoscope (a flexible tube with a light and camera at one end) is passed down into your stomach and lit up.
A small cut is made in your stomach where the light shines and the tube is then passed through. The operation usually takes around 20 minutes.
You will be in the unit for some time before and after the operation.
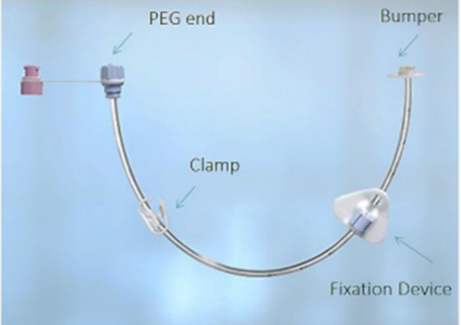
This is what a PEG tube looks like:
If you are having a PIGG
This is done in the Interventional Radiology Department. A narrow tube is passed through your nose into your stomach. Air will be passed into your stomach through the tube to make it visible on X-ray.
Local anaesthetic will numb your stomach. A small cut is made in your stomach and a wire is passed through to your mouth. The feeding tube is then passed through.
This operation typically takes 30 minutes.
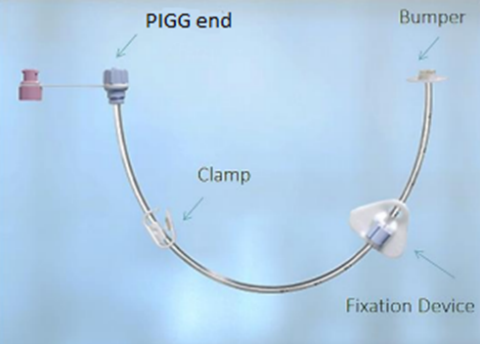
This is what a PIGG tube looks like:
If you are having a RIG
This is done in the Interventional Radiology Department. A narrow tube is passed through your nose into your stomach. Air will be passed into your stomach through the tube to make it visible on X-ray.
Local anaesthetic will numb your stomach and stitches are placed to hold the stomach close to the wall of the abdomen. A small cut is made near the stitches and a feeding tube is passed through into the stomach.
This operation typically takes 30 minutes.
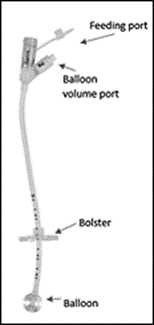
This is what a RIG tube looks like:
What happens afterwards?
- Once back on the ward it be 4-24 hours before you can use the tube. The nursing staff will tell you when you can start to use the tube.
- Water will be put through the tube first, followed by feed. Your dietitian will discuss the amounts and timings with you.
- The nutrition given through the tube is a prescribed liquid mix of the nutrition your body needs. We call this “specialist feed”. The specialist feed, water, and medications can be put down the tube using a special syringe or pump.
- You will need to sit upright during feeding and for 30-60 minutes afterwards.
- The dietitians will provide training on how to give the feeds and water flushes. This will be done as soon as possible so that you can go home quickly. Either the nursing staff on the ward or the community feeding team can provide further training.
After your tube has been inserted there is an increased risk of complications. If you are going home within 72 hours after the tube is inserted, you will need to be aware of these.
If there is:
- Leaking of fluid around the tube.
- Pain on feeding.
- Prolonged or severe pain after the operation.
- New bleeding.
Stop feed immediately
Phone your community feeding team or visit your local accident and emergency department for urgent advice
How do I look after my feeding tube?
PEG / PIGG
1-5 days after insertion
Once the tube is safe to use, you will begin to receive feed, medications, and water through the tube.
Flush the tube with water before and after you give the feed or medications to prevent the tube blocking
You should flush the tube with a minimum of 30mls of water every day if you are not giving nutrition or medications through the tube.
Clean the tube site (area where tube enters the skin) every with sterile water. Do this once or twice a day for the first 5 days.
After 5 days, use mild soapy water. Dry the area around the tube gently but thoroughly. Do not reposition the fixation device (triangle) unless advised.
Check for signs of pain, redness, swelling or leakage. Report any concerns to medical staff or the community feeding team.
The tube site doesn’t need a dressing after the first1-2 days. A simple gauze dressing can be used if there is leakage around the tube site.
2 weeks after insertion
Continue to clean the tube site including around the fixation device with mild soapy water and dry well.
2 weeks after insertion, or when the tube site has healed, it is important to prevent the overgrowth of skin around the tube inside the stomach. We call this ‘buried bumper’ syndrome.
To prevent a ‘buried bumper’, the tube needs to be moved daily. This is called “advancing and rotating” the tube. The dietitian will show you how to do this before you leave hospital. The community feeding team will also demonstrate this.
To “advance and rotate” the tube:
- Release the blue clip on the fixation device (triangle).
- Move the fixation device at least 4cm away from the stomach.
- With mild soapy water, clean both the tube site and the length of tube between the fixation device and stomach.
- Push 3-4cm of tube into the stomach.
- Turn the tube in a full circle (360 degrees).
- Pull the tube back until you feel some resistance.
- Wipe the tube clean.
- Place the fixation device approximately 5mm (pound coin width) from skin and close the blue clip. See Fig 6 and Fig 7 below.
This should only be done when the tube site is healed.
RIG
1-7 days after insertion
You shouldn’t eat or have anything via the tube for at least 4 hours after insertion.
You shouldn’t eat or have anything through the tube for at least 4 hours after insertion.
After this the tube will be flushed with 50ml of sterile water. If there are no concerns after 2-3 hours, then the tube is safe to use.
If there are signs of pain or leakage, let the nurse know.
You may have a dressing over the tube. The dressing should be changed every day for the first 7-10 days after insertion.
Clean the site every day with sterile water. You can lift the edges of the bolster (white circular disk) and clean underneath. Make sure the area around the tube is dried well.
Do not move the bolster for first 2 weeks after insertion.
Always check the marking where the bolster sits before putting anything through the tube. If there is a change in position of the tube do not use and contact the community feeding team immediately.
7-10 days after insertion
Some people like to keep a simple dressing on the tube but it is no longer needed.
Continue to clean the tube site with sterile water and dry well.
2 weeks after insertion
The stitches can be removed if they have not dissolved after 2 weeks. This can be done by the nutrition nurses.
The tube can be rotated daily once stoma tract has healed to prevent any overgrowth of skin. To do this, clean around the site with warm mild soapy water and dry well. Make sure you lift the edges of the bolster and clean underneath. Turn the tube in a full circle (360 degrees).
The water in the balloon should be changed 2 weeks after insertion and once a week after that. This is to make sure the balloon stays inflated to hold the tube in place.
In hospital, the ward dietitian or nurse will change the balloon water. You will be shown how to do this by the dietitian or community feeding team. When changing the balloon water, you can “advance and rotate” the tube at the same time. This helps prevents any overgrowth of skin on or around the tube.
To “advance and rotate” the tube:
- Make note of the mark on the tube where the bolster sits.
- Gently move the bolster away from the skin surface by at least 4cm.
- With mild soapy water, clean both the tube site and the length of tube between the bolster and stomach.
- Push 3-4cm of tube into the stomach.
- Turn the tube in a full circle (360 degrees).
- Pull the tube back until you feel some resistance.
- Wipe the tube clean.
- Place the bolster back to the original position approximately 5mm (pound coin width) from skin.
The tube needs to be changed around 3 months after insertion. This is usually done where you live by the community feeding team.
Further tube changes will usually be done every 3-6 months. If you wish, you or your carers can be trained to change the tube yourselves.
What help is available once I leave hospital?
Your ward dietitian will refer you to the community feeding team or an alternative service in your area. The community feeding team are known as the home management services (HMS).
The team comprises of dietitians, home enteral feeding nurses and a delivery company. They will contact you to arrange a monthly delivery of feeds and plastic equipment, such as syringes.
We may send you home from hospital with a small supply of feeds and equipment.
Your ward dietitian will explain your home feeding plan and provide contact details for the HMS team. Your GP may also be involved in the management of your tube.
What do I do if the tube becomes blocked?
Medicines can block the tube if they are not given correctly. You may need to be prescribed medicines in a more suitable form such as liquid. Your doctor or pharmacist should arrange this for you. Each medication should be given individually.
To help prevent tube blockage, we advise you do not give anything other than the feeds, water, and medications through your tube.
If you are unable to flush the tube or can see a blockage you should:
- Ensure all clamps are open and the tube is not bent.
- Massage the tube to try to dissolve any blockages.
- Flush with 50ml warm or soda water, leave for 30mins and re-flush. Never use pineapple juice, cola or lemonade as they can make the blockage worse.
- Try the ‘push/pull’ action with a syringe as advised by nursing staff.
- Contact community feeding team or call the 24 hour helpline on your feeding regimen.
Note: For a RIG tube, only trial these methods if the tube can be advanced and rotated. Otherwise, contact your community feeding team.
How long will I need the tube?
The tube can be removed if you no longer need it or want it removed. If well cared for can last several years.
The RIG tube will be changed every 3-6 months.
What if the tube is accidentally removed?
For PEG/PIGG tube
If the tube comes out you will need to go to your nearest accident and emergency department immediately. The longer the tube is out, the greater the risk of the site closing over.
For RIG tube
If your RIG tube comes out, ring the community feeding team or 24 hour helpline. You may need to go to your nearest accident and emergency department to have another tube inserted.
The community enteral feeding nurses may have trained you to insert a device into the stoma called Corstop ACE stopper or ENPlugs.
In the case of the tube coming out, you can insert this device. Then call the community feeding team or 24 hour helpline for further advice.
Common questions
Can I shower/bath?
You can shower from the day after the tube has been placed. Do not have a bath for at least 4 weeks until the area around the tube has healed. Make sure the end is closed and clamp applied before washing. Fully dry the area around the tube after.
Can I swim?
Only once the area around the tube has healed. Use a waterproof dressing. Fully dry the area around the tube after.
Can I go on holiday?
The tube does not stop you going on holiday. You may need to take a GP letter and insurance documents with you. Contact the home feeding team for further information.
Will I be able to move freely?
The tube should not restrict your everyday activities. You can cover the tube with loose clothing.
What happens if I become unwell?
If you feel unwell and are unable to give yourself your feed, it is important to keep hydrated. Flush the tube regularly with water to prevent the tube blocking and to keep hydrated. Speak to your GP, nurse or dietitian if you are concerned.
How do I keep my mouth clean?
You will need to keep your mouth and teeth clean by brushing regularly. This is important even if you cannot eat and drink. A mouthwash and artificial saliva spray may help to keep your mouth moist. The speech and language therapist can guide you on this.
Who pays for the feeds?
If you are an NHS patient and registered with a GP, your local health authority will pay for the feeds.
What do I do if I experience any pain, discomfort or issues with my tube site?
If you experience any pain or discomfort then stop any feed. Contact the community feeding team for further advice. Contact the community feeding team if the skin around the site becomes red and sore or if there is oozing or bleeding.
Further information
Nutricia website provides information on specialist feed and using a feeding pump. There is also information on the nursing team who help people with feeding tubes:
PINNT helps people on enteral and parenteral nutrition providing advice and local help groups.
- Phone 020 3004 619
- PINNT: Advocacy & support for people on home artificial nutrition (HAN): parenteral, enteral & oral nutritional supplements. | PINNT
References
- Arvanitakis, M., Gkolfakis, P., Despott, E., Ballarin, A., Beyna, T., Boeykens, K., Elbe, P., Gisbertz, I., Hoyois, A., Mosteanu, O., Sanders, D., Schmidt, P., Schneider, S. and van Hooft, J., 2020. Endoscopic management of enteral tubes in adult patients – Part 1: Definitions and indications. European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy, 53(01), pp.81-92.
- Gkolfakis, P., Arvanitakis, M., Despott, E., Ballarin, A., Beyna, T., Boeykens, K., Elbe, P., Gisbertz, I., Hoyois, A., Mosteanu, O., Sanders, D., Schmidt, P., Schneider, S. and van Hooft, J., 2020. Endoscopic management of enteral tubes in adult patients – Part 2: Peri- and post-procedural management. European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy, 53(02), pp.178-195.
- Nutricia Homeward (2021) Balloon Gastrostomy Tube Advice.
- Potack, Z. and Chokhavatia, S., 2008. Complications and controversies associated with Percutaneous Endoscopic Gastronomy. Report of a Case and Literature Review. The Medscape Journal of Medicine, 10(6), pp. 142.
- Toussaint, E., Van Gossum, A., Ballarin, A. and Arvanitakis, M., 2015. Enteral access in adults. Clinical Nutrition, 34(3),pp. 350-358.
© North Bristol NHS Trust. This edition published October 2024. Review due October 2027. NBT002346.
